What is SIFO? Is it a Mast Cell Trigger like Mold?
My GI issues had just started turning the corner – I was so excited to be eating more foods without having intense gut pain!
Unfortunately, all of a sudden, I started having diarrhea again. The pain was ramping back up.
Sadly, even my food intolerances started coming back. I was feeling so discouraged.
But I knew I could figure it out with some detective work. I hadn’t changed anything in the past 3 months, so what could it be?
A clue finally emerged – my gut pain worsened when I drank the hydrogen water from this fancy machine I was testing. This seemed strange since I had used it before without any problems.
But then I remembered I’d sent the machine off for some repairs. The company said they would drain the machine of water entirely and sanitize it before sending it back to me.
But when I was looking for clues as to why I was feeling sick again, I realized my issues started soon after I got the machine back.
So, I tested the water with mold plates.
The hydrogen machine came back with high levels of both mold and bacteria – YUCK!!
I had literally been drinking mold and bacteria for several weeks. (Spoiler alert: I don’t use this machine anymore!)
Before I’d seen the water testing results though, I figured my gut issues were from SIBO (small intestinal bacterial overgrowth.)
So, I did an Elemental Diet to get rid of it. But a week in, my diarrhea became severe.
This is the opposite of what should have happened with an Elemental Diet!
Between the Elemental Diet issues and the mold plate results, it dawned on me that I had both SIBO and SIFO (small intestinal fungal overgrowth).
And then testing confirmed my suspicions – a number of the gut fungal markers were elevated!
The Elemental Diet can work very well for SIBO.
But the Elemental Diet can worsen SIFO. And I was definitely getting worse.
If I had done the Elemental Diet while taking antifungals, I would have been better off.
What I later found out was that SIBO and SIFO often occur together in people with Mold Toxicity. (Which I also had!)
And SIBO, SIFO, and Mold Toxicity are all mast cell triggers. It’s no wonder I felt so sick!
Have you had unexplained gut issues, too?
Not everyone with SIBO or SIFO gets diarrhea. Some people get constipation instead. And others can alternate between loose stools and constipation.
There are lots of other symptoms, too. I’ll share those with you in just a bit. But first, what exactly is SIFO?
Keep reading to learn more about:
- What is SIFO?
- SIFO, SIBO, and Mold Toxicity
- Is SIFO common?
- Causes of SIFO
- Symptoms of SIFO
- SIFO and its effects on mast cells
- Testing for SIFO
- How to get rid of SIFO
Let’s start by answering the question:
What is SIFO?
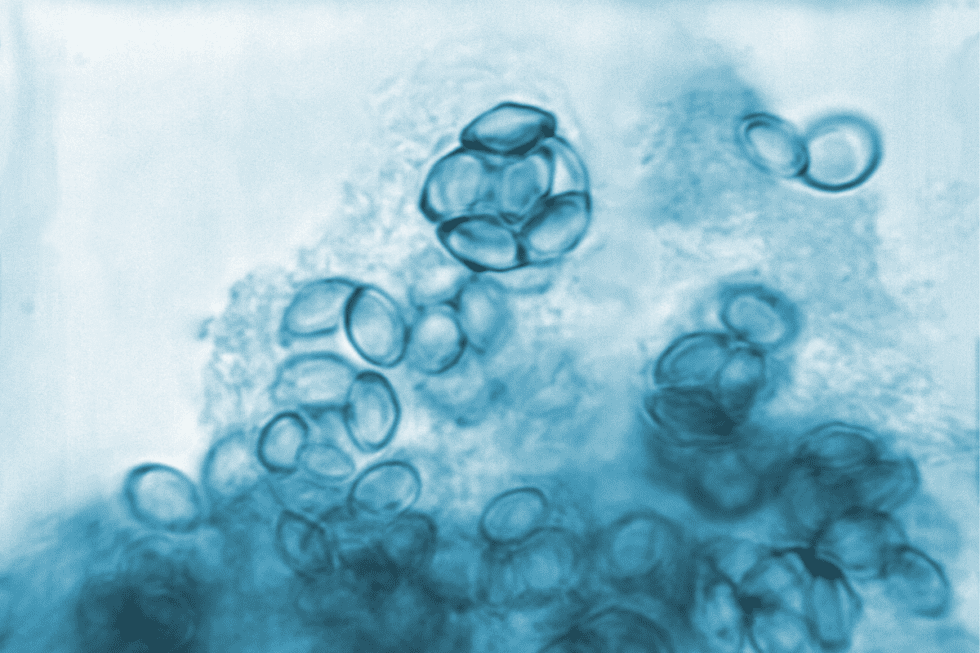
The name suggests that SIFO (small intestinal fungal overgrowth) is an overgrowth of fungus. In a way, this can be true.
But it may be more accurate to say that it is a fungal imbalance in the gut. An imbalance will often mean overgrowth, though. So, you may just hear it referred to as overgrowth.
The two most common culprits behind SIFO are
- Candida (a yeast which is a type of fungus)
- Mold Colonization in the gut
First, let’s look at SIFO from Candida.
Candida is the fungus most commonly studied in relation to SIFO.
Candida albicans is one type of fungus naturally found in your gut. This is the scientific name for what you probably know as simply Candida.
Now, everyone has a small amount of Candida in their gut. This is normal. It’s when there is an overgrowth of Candida that problems begin to happen.
When I got SIFO from the hydrogen water machine, it wasn’t my first run-in with fungal issues in my body.
When I had them before, I had tell-tale signs for a couple decades before I knew what was going on.
I had issues like:
- Terrible GI issues
- Vaginal yeast infections
- Dark patches of skin in my groin area
- White coating on a cracked tongue
- Sinus congestion and postnasal drip
- Thick, yellow toenails
- Bad sugar and carb cravings
But when I had SIFO and these other fungal issues before, the practitioners misdiagnosed me with systemic Candida overgrowth.
Candida was only one part of the problem.
So, if you have SIFO from other types of fungal species, addressing Candida alone may not do much to help your symptoms.
For example, molds like aspergillus or fusarium are different types of fungi that can lead to SIFO. And you don’t deal with them in the same way you deal with Candida
In my case, my symptoms never cleared up no matter how hard I worked on getting rid of the Candida.
And it was because the doctors I saw were missing that mold was underlying all my symptoms!
I had all kinds of issues related to mold. SIFO ended up being one of them.
The kinds of SIFO I see a lot in those with MCAS aren’t as commonly known about. And if you bring up SIFO, many times you’ll get strange looks or possibly be dismissed.
But it may be much more common than previously thought.
2 studies were recently done on a test group of patients with unexplained GI symptoms. Results showed about 25% of the subjects had SIFO.
And SIFO may be more common among people who:
- Have Mold Toxicity
- Have Diabetes
- Have motility issues in which gut muscles aren’t pushing food through the small intestine properly
- Are taking PPIs, steroids, or antibiotics
- Low stomach acid
- Have weakened immune systems
But Candida isn’t the only fungal issue that can cause SIFO.
Mold Colonization in the gut happens a lot, too. It’s just not being talked about or studied enough yet.
Let’s look at Mold Colonization and SIFO next.
SIFO from Mold Colonization
Unlike Candida, mold shouldn’t be growing in the gut at all. I’m talking about mold species like aspergillus or fusarium. These molds can colonize in the gut and create tons of problems.
Here’s how Mold Colonization in your gut can happen.
First, you need exposure to mold.
Have you been exposed to mold for several weeks or longer? If so, you might have inhaled mold spores.
Mold reproduces by spreading spores. These spores can get into the air that you breathe.
Think of a fluffy, white dandelion blowing in the wind. Mold spores spread through the air kind of like that except you never see them. They’re microscopic.
So, when you breathe in mold spores, they can make their way into your sinuses. Then these spores can move through your body in mucous made in the sinuses.
Here’s one way mold spores can get from your sinuses to your gut.
At some point, you’ve probably experienced post-nasal drip. It happens to all of us. This is where mucous from the nose drains down the throat.
So, you end up swallowing this mucous containing mold spores.
Mold spores can also get in your gut by landing in your food and drinks. In areas where there are a lot of mold spores in the air, this can happen.
That’s how mold spores get in your body. And if these mold spores take hold and grow, mold will actually start growing in your body. That’s Mold Colonization.
Mold Colonization can be a two-fold problem. First, it can result in Mold Toxicity.
Mold Toxicity is what happens when you get ill (often chronically ill) from toxins made by mold. These toxins are called mycotoxins.
And when mold is growing inside you, that means more mold toxins are being released from that mold inside your body. You’ll feel even sicker.
You can actually have Mold Toxicity and not Mold Colonization. But if you have Mold Colonization, you are almost always going to have Mold Toxicity.
Mold Toxicity can cause serious health issues. But you can have Mold Toxicity and not have SIFO.
However, if you have Mold Colonization in your gut, that’s likely going to create the perfect conditions for SIFO to flourish.
And here’s where it gets really bad if you have Mast Cell Activation Syndrome.
Mold and Mast Cells
Mold releases all kinds of enzymes (like proteases and hydrolyses) to break down your body’s tissue.
Mold needs to break your body down so it can feed on the nutrients in your tissue!
Mold decomposes your body the same way it uses these same enzymes to decay a piece of fruit or bread.
What does this mean if you have Mast Cell Activation Syndrome? Your mast cells are major responders to mold. They are also responders to injury.
Your mast cells will be triggered by mold AND your mast cells will see this decomposition of your tissues as a type of injury.
You’ll end up with a lot more mast cell activation which can lead to all kinds of reactions.
Next, let’s look at more connections between mold, SIFO, SIBO and MCAS.
Mold’s Role in SIFO, SIBO, and Mast Cell Activation Syndrome
A healthy immune system should be keeping both bacterial and fungal species in check.
But mold toxins weaken the part of the immune system that should keep bacteria and yeasts (fungus) from overgrowing.
And mold sets up extra protection for itself once it’s in your body.
It disrupts your system in a way that keeps your immune system from attacking mold spores!
Oxalates are another part of this picture.
Certain molds can produce oxalates when colonized in you. Candida feeds off oxalates. That means even more Candida growth.
So, it’s no wonder that mold exposure is one of the most common root causes for both SIBO (small intestinal bacterial overgrowth) and SIFO (small intestinal fungal overgrowth).
In fact, a weakened immune system makes it hard to keep any kind of virus, bacteria, or mold in check.
That means if you have Mold Toxicity, it’s also more likely you’ll get viruses like Epstein Barre (EBV) and tickborne infections like Lyme.
When I had SIFO the first time (before the water machine disaster), I hadn’t addressed detoxing mold yet.
Since that time, I had started to work on detoxing mold.
I was starting to feel much better, but I wasn’t fully recovered. My immune system was still considerably weakened from the mold.
It made me more vulnerable to get both SIBO and SIFO when I was exposed to bacteria and mold from the water machine.
I truly hope you don’t ever have to go through this once, let alone twice!
But if you do find yourself with SIFO, I’ll give you some ideas for how to get rid of it later on in this post.
To Review
- SIBO is bacterial overgrowth in the small intestine
- SIFO is fungal overgrowth in the small intestine.
- Mold produces toxins that weaken the immune system
- Mold Toxicity increases your risk for developing both SIFO and SIBO
- Mold Colonization (like aspergillus or fusarium) in the small intestine can lead to SIFO
- Mold Toxicity and Colonization can lead to Mast Cell Activation
- Mold Colonization can worsen Candida
- Mold produces oxalates and Oxalates feed Candida which encourages growth
- Mold in the gut is likely a much worse condition than SIBO or Candida – it isn’t being studied or taken seriously enough
- Mold Colonization in the gut needs to be addressed in order to clear up your SIBO or Candida
Basically, mold is bad news all around.
In addition to mold, there are other factors that can lead to an increased risk for developing SIFO.
Let’s look at those next.
Other Risk Factors for Developing SIFO
While mold exposure is a big reason you can develop SIFO, there are other things that can contribute, too.
Do any of these apply to you?
- Are you taking any PPIs or steroids?
- Do you eat a lot of sugar or carb foods?
- Do you have immune conditions?
- Do you have low stomach acid?
All these things can make it more likely for you to develop SIFO.
Let’s take a look at each of these.
Diet
A diet high in sugar and refined carbohydrates is perfect food for feeding fungal species like yeast and molds.
These get converted to glucose in your body. Yeast and molds love glucose.
High blood sugar is also another risk factor for Candida and mold growth in your body.
Eating multiple small meals plus snacks throughout the day can be problematic in SIFO (and SIBO). Here’s why.
Your gut needs time to rest. When it rests, it goes into repair mode. And this happens only if it isn’t putting energy into digestion. You can also think of this as clean out mode.
It’s during this time that your gut also gets rid of residual undigested material. If that material sits around because your gut never has time to sweep it out, it creates a perfect food source for bacteria and fungi.
Not only can fungi and bacteria thrive on waste matter, they can feed on the food you eat, too. So if you are constantly eating, you’re constantly providing food for these microorganisms to eat, too.
Now, you always want to make sure you are getting enough to eat and getting a variety of nutrients from as many foods as you can tolerate.
But some people are able to start spacing out their meals or reduce their snacking, which can help their gut. This isn’t right for everyone, so be sure to work with your health care practitioner.
Motility Issues
In a 2013 study, just over half of the participants with SIFO from Candida also had GI motility issues.
In particular, slow motility is a problem. You can actually have slow motility in the small intestine with either constipation or diarrhea.
Slow motility means the muscles in your gut aren’t moving food through efficiently. So, food sits in your small intestines longer.
This means more opportunities for bacteria and fungi to feed and get imbalanced or grow out of control.
Stomach Acid and PPIs
Healthy levels of stomach acid can help prevent SIFO issues. For one, stomach acid is needed for digestion.
It helps break your food down so you can digest it more quickly. This means less sitting in the small intestine to feed Candida and molds.
But stomach acid is also needed to kill off mold spores that get swallowed before they enter your intestines.
You can have low stomach acid from:
- Age
- Dysregulated nervous system
- Chronic Stress
- Infections
- Surgeries
- Medications
In particular, you can have low stomach acid from PPI (proton pump inhibitor) medications.
If you have acid reflux or GERD, you might be taking a PPI. But this can lead to even lower stomach acid opening you up to more problems.
Important Tip: H2 blockers like Pepcid are different from PPIs. H2 blockers are often helpful in MCAS. These don’t cause the serious stomach acid issues seen in PPIs.
However, if you have extremely low stomach acid and get heartburn from H2 blockers, you may need to work on your stomach acid first.
Antibiotics
Antibiotics are another type of medication that can contribute to SIFO. Taking antibiotics can disrupt the gut microbiome (this just means organisms in the gut).
In a healthy, balanced microbiome, beneficial bacteria and beneficial yeasts help keep Candida and mold in check.
Antibiotics can kill off both the good and bad bacteria. When good bacteria die off, there’s nothing to fight off the fungal species.
This is how chronic antibiotic overuse can lead to SIFO (and SIBO).
Immune Deficiencies
If your immune system is compromised, it can be harder to fight off any type of infection, including fungal overgrowth. Remember, we talked earlier about how mold compromises your immune system.
Mold is one thing that can lead to immune deficiencies. There can be many others.
Regardless of what has caused your immune deficiency, it may impair your ability to fight off infections like SIFO.
Now you know what leads to SIFO. But what are the symptoms?
Keep reading to learn more.
Symptoms of SIFO
Here are some of the more common symptoms of SIFO. Count how many you have.
Do you suffer from any of these gastrointestinal or gut symptoms?
- belching
- bloating
- diarrhea
- constipation
- gas
- indigestion
- nausea
You might even mistake this for IBS or irritable bowel syndrome. Many symptoms are the same.
But have you tried addressing your symptoms for IBS? Were you successful?
If not, take a look at some of these other symptoms and conditions related to SIFO. Do you have any of the following?
Nervous system symptoms like:
- migraines
- fatigue
- depression
And here are some other indicators you might have SIFO. How many of these apply to you?
- Do you have sugar and carb cravings?
- Frequent sinus infections or congestion?
- Do you have dandruff? (fungal overgrowth of the scalp)
- Do you have athlete’s foot?
- Toenail fungus?
- Tinea versicolor? (fungal infection of skin leading to light or dark patches)
- Jock itch for men or frequent vaginal yeast infections for women?
- Itchy ears?
- Yeasty smell in armpits, groins, genitals, or under breast tissue?
- White coating on tongue (thrush)?
If you answered yes to most of these questions, it might be time to look more into SIFO.
If you answered yes to only a couple, don’t rule SIFO out yet.
It could be SIFO, but it may also be a more localized fungal infection instead of all over your body.
Either way, be sure to talk with your health practitioner.
How Can You Test For SIFO?
First, you want to be sure to rule out other conditions. And of course, be sure to talk with your provider if you have new or worsening symptoms of any kind.
If you and your healthcare provider have ruled out other conditions, there are ways you can detect SIFO. It can be challenging, though.
There aren’t any simple, easy tests. But, let’s look at what is available.
The only definitive testing for SIFO currently is an invasive procedure.
This procedure is done with what’s called a small bowel or duodenal aspirate. This involves removing digestive fluids from a part of the small intestine called the duodenum. This fluid is then cultured to look for mold and Candida growth.
Duodenal aspirate testing is rarely done though. It’s too invasive. And SIFO still isn’t taken seriously enough.
If you suspect SIFO, you can consider looking at other types of testing for clues.
Like I said, the invasive procedure is the only definitive testing. However, the following 2 tests might provide you with some helpful data.
Here are 2 tests you can get yourself:
Great Plains mOAT (microbial Organic Acids Test)
This is a urine test. You don’t even need a healthcare provider to order it for you.
>>> US can order the Great Plains mOAT directly here
>>> Canadians can order the Great Plains mOAT directly here
The mOAT (microbial organic acids test) has 9 markers for yeast and mold overgrowth. If one of these is positive, you very likely have SIFO.
It can miss SIFO though.
This is because it’s only possible right now to do a urine test for a small handful of fungal markers out of the hundreds of possibilities.
What that means is that if this test comes back negative it doesn’t necessarily rule out SIFO.
It just means that other markers that can show mold or Candida weren’t tested for.
But if this test comes back positive, you’ll know you are dealing with SIFO.
GI 360
This is a stool test that includes testing for Candida. I prefer the 3-day version to get a more thorough picture.
You can also order this directly without needing a healthcare provider.
Like the mOAT, this isn’t definitive because it is looking at what’s happening in your large intestine.
By the time Candida shows up in a stool test, there is a very large load of Candida present in your system.
If this comes back positive, it can be a good indicator that you have Candida overgrowth in your gut.
What if these are negative but you still suspect SIFO?
Now, let’s say you got both tests done and both were negative. This happens sometimes.
You want to then ask yourself – have you had a lot of mold exposures?
If so, you and your practitioner may need to go by symptoms and your health history to decide if you likely have SIFO.
So, what can you do to get rid of SIFO? I’m sure you’re ready to be done with the bloating, belching, abdominal pain, and constipation or diarrhea!
I certainly was! Let’s look at some of the very beginning steps you can consider next.
Getting Rid of SIFO
First, you have to address the root issues.
Is your SIFO coming from any of these:
- Still being exposed to mold?
- Mold Colonization that hasn’t been addressed?
- High carbs and sugars?
- Uncontrolled blood sugar?
- Eating too often?
- GI motility issues?
- Low stomach acid?
- PPIs, steroids, or antibiotics?
You may need a skilled practitioner to help you in working with these root causes.
If you have multiple factors, the first place to start is getting away from mold exposures as much as possible.
I can’t say it enough:
Get Out of Mold
Getting out of mold is very likely going to do wonders for improving your health.
If you aren’t constantly inhaling or ingesting new spores, you can detox mold and start to recover your health.
But even if you can’t get out of mold right away, there are other things you can do to help start getting SIFO under control.
Start with What you Eat
Cut back on refined carbohydrates and avoid sugar. Unless contraindicated like with porphyria, of course.
Space meals out if possible. This helps with something called the migrating motor complex (MMC).
The MMC works to clean out the small intestine. MMC kicks in when the body isn’t digesting. Spacing out meals gives you time to digest, and time for the MMC to clean up.
Consider Supplements and Antifungals
In some cases, you may need a medical practitioner to prescribe antifungals to start addressing fungal overgrowth.
But you can also consider these gentle starting points.
Saccharomyces Boulardii
Did you know there is actually beneficial yeast? It’s a type of probiotic. It’s low oxalate, no salicylates.
It has a lot of benefits. By being a beneficial yeast, it can outcompete mold and Candida.
The cell wall of this beneficial yeast also works as a binder. It helps to remove certain mycotoxins (mold toxins) like gliotoxin, aflatoxin, and zearalenone from your body.
It’s also been shown to enhance antifungals. So, if you are taking antifungals, you can consider adding this to get the most out of them.
One study found Saccharomyces Boulardii to be as effective in infants as nystatin (a common antifungal).
However, it may not be tolerated if you have Candida IgE or IgG antibodies. This is because both Saccharomyces and Candida are in the same yeast family.
This means, even though Saccharomyces Boulardii probiotic is beneficial, people with Candida allergies may have trouble with it until the allergies are cleared up.
If you aren’t sure, start with little sprinkles and build up slowly as tolerated.
You can also get 15% off anything at Fullscript anytime when you register with this link. If you don’t have an account already, it’s free and you just enter your email address to sign up. It never costs you any more, but your Fullscript purchase helps support Mast Cell 360 free online resources.
Tulsi Tea or Tincture aka Holy Basil
Tulsi contains high levels of a compound called eugenol. Eugenol may help fight bacteria and molds.
It’s low oxalate, but contains salicylates.
You want to use really fresh, organic options for this. This is because it’s the essential oils that contain the eugenol.
Those essential oils can evaporate over time if the Tulsi isn’t fresh. Most herbal teas are between 6 months to over a year old by the time they hit the shelf at the grocery store!
The best and most effective option I’ve found is from Kauai Farmacy. They make both a tea and a tincture version.
>>>>You can use coupon code mastcell360 for 15% off.
If you’re extremely sensitive, you can consider starting with 1 cup of tea per day and working up to 4 or 5 cups per day if possible.
If you are moderately sensitive, you could try 1 drop of the tincture in water per day. (Tinctures are more concentrated.)
As tolerated, you could consider increasing slowly to 2-3 dropperfuls of tincture 2x/day.

Argentyn 23 Silver Oral
This is another option to consider. It’s been shown to inhibit Candida, mold, and bacteria.
It has no oxalates and no salicylates.
But if you are also taking the beneficial yeast S. boulardii, Argentyn 23 won’t compromise it.
Argentyn 23 also penetrates biofilm. Biofilms are protective coverings that Candida mold produces to keep itself safe from treatments.
If you can get past that layer, you can address mold more efficiently.
Tip: DON’T use colloidal silver. This is a higher particle size that can build up in your body and cause serious problems. Argentyn 23 is a nanoparticle silver that is at the parts per billion size – this means it’s so small it can’t build up in your tissues.
Argentyn 23 was shown in a study to be the most effective of the silver compounds.
One way to take Argentyn 23 silver oral is to start with 1 drop and increased very slowly to ½ tsp 2x/day. Hold under tongue for 30 seconds.
These 3 things are very gentle starting points. If you’re dealing with SIFO and Mold Toxicity, you’ll probably need a more comprehensive and individualized approach.
Are you ready for more? If so, check out the Advanced Mold Course for this in-depth information.
Have you dealt with SIFO? What worked for you? We’d love for you to share in the comments below!
What to Read Next
- Lyme, SIBO, Candida, EBV in Mold Toxicity – Why won’t they go away? What do you do to get rid of them?
- 7 Most Common Detox Mistakes Made by Sensitive People – What to Know When You Have Mast Cell Activation Syndrome and Histamine Intolerance
- Testing Mycotoxins and Mold: One of the Biggest Root Triggers for Mast Cell Activation | Histamine Intolerance
- Could You Have SIBO and Histamine Intolerance and/or Mast Cell Activation Syndrome?
- SIBO Diet, Lifestyle Changes, and Supplements for MCAS and HIT
Some links in this website are affiliate links, which means Mast Cell 360 may make a very small commission if you purchase through the link. It never costs you any more to purchase through the links, and we try to find the best deals we can. We only recommend products that we love and use personally or use in the Mast Cell 360 practice. Any commissions help support the newsletter, website, and ongoing research so Mast Cell 360 can continue to offer you free tips, recipes, and info. Thank you for your support!
References
Alassane-Kpembi, I., Puel, O., & Oswald, I. P. (2015). Toxicological interactions between the mycotoxins deoxynivalenol, nivalenol and their acetylated derivatives in intestinal epithelial cells. Archives of toxicology, 89(8), 1337–1346. https://doi.org/10.1007/s00204-014-1309-4
Armando, M.R., et al. “Adsorption of Ochratoxin A and Zearalenone by Potential Probiotic Saccharomyces Cerevisiae Strains and Its Relation with Cell Wall Thickness.” Journal of Applied Microbiology, vol. 113, no. 2, 2012, pp. 256–264., doi:10.1111/j.1365-2672.2012.05331.x.
Ash, M. (2018, July 12). The Role of HCL In Gastric Function And Health. Clinical Education. https://www.clinicaleducation.org/resources/reviews/the-role-of-hcl-in-gastric-function-and-health/
Bankova, L. G., Lai, J., Yoshimoto, E., Boyce, J. A., Austen, K. F., Kanaoka, Y., & Barrett, N. A. (2016). Leukotriene E4 elicits respiratory epithelial cell mucin release through the G-protein-coupled receptor, GPR99. Proceedings of the National Academy of Sciences of the United States of America, 113(22), 6242–6247. https://doi.org/10.1073/pnas.1605957113
Bhagatwala, J., & Rao, S. S. C. (2020). Small intestinal bacterial and fungal overgrowth. Clinical and Basic Neurogastroenterology and Motility, 343–358. doi:10.1016/b978-0-12-813037-7.00024-8
Brewer, J H., Hooper, D., Muralidhar, S., (2015). Intranasal antifungal therapy in patients with chronic illness associated with mold and mycotoxins: an observational analysis. Global Journal of Medical Research, 15(1).
CLELAND, W. W., & JOHNSON, M. J. (1956). Studies on the formation of oxalic acid by Aspergillus niger. The Journal of biological chemistry, 220(2), 595–606.
Conti, P., Tettamanti, L., Mastrangelo, F., Ronconi, G., Frydas, I., Kritas, S. K., Caraffa, A., & Pandolfi, F. (2018). Impact of Fungi on Immune Responses. Clinical Therapeutics, 40(6), 885–888. https://doi.org/10.1016/j.clinthera.2018.04.010
Demirel, G., Celik, I. H., Erdeve, O., Saygan, S., Dilmen, U., & Canpolat, F. E. (2013). Prophylactic Saccharomyces boulardii versus nystatin for the prevention of fungal colonization and invasive fungal infection in premature infants. European journal of pediatrics, 172(10), 1321–1326. https://doi.org/10.1007/s00431-013-2041-4
English, J. (2018, November 25). Gastric Balance: Heartburn and Gastritis Not Always Caused by Excess Acid. Nutrition Review. Retrieved March 30, 2022, from https://nutritionreview.org/2018/11/gastric-balance-heartburn-and-gastritis-not-always-caused-by-excess-acid/
Erdoğan, A., Lee, Y.Y., Sifuentes, H., & Rao, S.S. (2014). Sa2026 Small Intestinal Fungal Overgrowth (SIFO): A Cause of Gastrointestinal Symptoms. Gastroenterology, 146.
Erdogan, A., & Rao, S. S. (2015). Small intestinal fungal overgrowth. Current gastroenterology reports, 17(4), 16. https://doi.org/10.1007/s11894-015-0436-2
Fuji, S. (2016, December 12). Hyperglycemia as a possible risk factor for mold infectionsâthe potential preventative role of intensified glucose control in allogeneic hematopoietic stem cell transplantation. Nature. https://www.nature.com/articles/bmt2016306&code=9db861f8-41cc-4d0c-a128-0f48ee87fc23
Goktas, H., Dertli, E., & Sagdic, O. (2021, January 1). Comparison of functional characteristics of distinct Saccharomyces boulardii strains isolated from commercial food supplements. ScienceDirect. https://www.sciencedirect.com/science/article/abs/pii/S0023643820313293
Guerra, J. D., Sandoval, G., Avalos-Borja, M., Pestryakov, A., Garibo, D., Susarrey-Arce, A., & Bogdanchikova, N. (2020, July 1). Selective antifungal activity of silver nanoparticles: A comparative study between Candida tropicalis and Saccharomyces boulardii. ScienceDirect. https://www.sciencedirect.com/science/article/abs/pii/S2215038220300601
Hallen-Adams, H. E., & Suhr, M. J. (2017). Fungi in the healthy human gastrointestinal tract. Virulence, 8(3), 352–358. https://doi.org/10.1080/21505594.2016.1247140
Jacobs, C., Coss Adame, E., Attaluri, A., Valestin, J., & Rao, S. S. (2013). Dysmotility and proton pump inhibitor use are independent risk factors for small intestinal bacterial and/or fungal overgrowth. Alimentary pharmacology & therapeutics, 37(11), 1103–1111. https://doi.org/10.1111/apt.12304
Jeziorek, M., Frej-Mądrzak, M., & Choroszy-Król, I. (2019). The influence of diet on gastrointestinal Candida spp. colonization and the susceptibility of Candida spp. to antifungal drugs. Roczniki Panstwowego Zakladu Higieny, 70(2), 195–200. https://doi.org/10.32394/rpzh.2019.0070
Kelesidis, T., & Pothoulakis, C. (2012). Efficacy and safety of the probiotic Saccharomyces boulardii for the prevention and therapy of gastrointestinal disorders. Therapeutic advances in gastroenterology, 5(2), 111–125. https://doi.org/10.1177/1756283X11428502
Khadivi, R., Razavilar, V., Anvar, A., & Akbari Adreghani, B. (2020). Aflatoxin M1-Binding Ability of Selected Lactic Acid Bacteria Strains and Saccharomyces boulardii in the Experimentally Contaminated Milk Treated with Some Biophysical Factors. Archives of Razi Institute, 75(1), 63–73. https://doi.org/10.22092/ari.2019.123985.1265
Krasowska, A., Murzyn, A., Dyjankiewicz, A., ŁUkaszewicz, M., & Dziadkowiec, D. (2009, December 1). The antagonistic effect of Saccharomyces boulardii on Candida albicans filamentation, adhesion and biofilm formation. OUP Academic. https://academic.oup.com/femsyr/article/9/8/1312/520904?login=true
Kritas, S. K., Gallenga, C. E., D Ovidio, C., Ronconi, G., Caraffa, A. l., Toniato, E., Lauritano, D., & Conti, P. (2018). Impact of mold on mast cell-cytokine immune response. Journal of biological regulators and homeostatic agents, 32(4), 763–768.
Kritas, S. K., Gallenga, C. E., D Ovidio, C., Ronconi, G., Caraffa, A. l., Toniato, E., Lauritano, D., & Conti, P. (2018). Impact of mold on mast cell-cytokine immune response. Journal of biological regulators and homeostatic agents, 32(4), 763–768.
Kunyeit, L. (2020, September 25). Application of Probiotic Yeasts on Candida Species Associated Infection. MDPI. https://www.mdpi.com/2309-608X/6/4/189/htm
Latifah-Munirah, B., Himratul-Aznita, W. H., & Mohd Zain, N. (2015, July 15). Eugenol, an essential oil of clove, causes disruption to the cell wall of Candida albicans (ATCC 14053). Taylor & Francis. https://www.tandfonline.com/doi/full/10.1080/21553769.2015.1045628
Lieberman, S. M., Jacobs, J. B., Lebowitz, R. A., Fitzgerald, M. B., Crawford, J., & Feigenbaum, B. A. (2011). Measurement of mycotoxins in People with chronic rhinosinusitis. Otolaryngology–head and neck surgery: official journal of American Academy of Otolaryngology-Head and Neck Surgery, 145(2), 327–329. https://doi.org/10.1177/0194599811403891
Liew, W. P., & Mohd-Redzwan, S. (2018). Mycotoxin: Its Impact on Gut Health and Microbiota. Frontiers in cellular and infection microbiology, 8, 60. https://doi.org/10.3389/fcimb.2018.00060
Mayer, F. L., Wilson, D., & Hube, B. (2013). Candida albicans pathogenicity mechanisms. Virulence, 4(2), 119–128. https://doi.org/10.4161/viru.22913
Nathan, N. (2018). Toxic: Heal Your Body from Mold Toxicity, Lyme Disease, Multiple Chemical Sensitivities, and Chronic Environmental Illness. Las Vegas: Victory Belt Publishing.
Piliponsky, A. M., & Romani, L. (2018). The contribution of mast cells to bacterial and fungal infection immunity. Immunological reviews, 282(1), 188–197. https://doi.org/10.1111/imr.12623
Pizzorno, J., & Shippy, A. (2016). Is Mold Toxicity Really a Problem for Our People? Part 2-Nonrespiratory Conditions. Integrative medicine (Encinitas, Calif.), 15(3), 8–14.
Poloni, V. L., Bainotti, M. B., Vergara, L. D., Escobar, F., Montenegro, M., & Cavaglieri, L. (2021). Influence of technological procedures on viability, probiotic and anti-mycotoxin properties of Saccharomyces boulardii RC009, and biological safety studies. Current Research in Food Science, 4, 132–140. https://doi.org/10.1016/j.crfs.2021.02.006
Ratnaseelan, A. M., Tsilioni, I., & Theoharides, T. C. (2018). Effects of Mycotoxins on Neuropsychiatric Symptoms and Immune Processes. Clinical therapeutics, 40(6), 903–917. https://doi.org/10.1016/j.clinthera.2018.05.004
Shaw, W., & Pratt-Hyatt, M. (2019). Biochemical Markers in the Urine Associated with Gastrointestinal Mold-Overgrowth Are Linked with Elevated Urinary Mycotoxins in Patients with Suspected Mold Illness. Townsend Letter, 31–38. https://www.townsendletter.com/article/436-biochemical-markers-urinary-mycotoxins-mold-overgrowth/
Suchodolski, J. (2021, March 22). Capric acid secreted by Saccharomyces boulardii influences the susceptibility of Candida albicans to fluconazole and amphotericin B. Nature. https://www.nature.com/articles/s41598-021-86012-9?error=cookies_not_supported&code=525c2f41-c0bf-4f6a-8205-20a8cf4de239
The Institute for Functional Medicine. (2021, July 23). SIBO: Comorbidities, SIFO, and Diagnosis. Retrieved March 25, 2022, from https://www.ifm.org/news-insights/microbiome-treating-sibo-and-its-comorbidities/
Urb, M., Pouliot, P., Gravelat, F. N., Olivier, M., & Sheppard, D. C. (2009). Aspergillus fumigatus induces immunoglobulin E-independent mast cell degranulation. The Journal of infectious diseases, 200(3), 464–472. https://doi.org/10.1086/600070




Thanks Beth. Your articles get better every year. I’m 99% I have SIBO or SIFO. I go between loose and nothing, and I am bloated like a balloon. It’s silly. I weight 115 lbs but look like I weigh 140. My sister has been treating SIBO and EBV, Yeast for 15 years. Now she found out she has MS.
Thank you so much! I’m glad to hear the articles have been helpful! I’m sorry to hear about your sister’s diagnosis, too, but hope that at least the diagnosis will help her understand what is going on for her and allow her to get the help she needs. Wishing you both the very best!
Interesting. I have looked high and low for info for SIFO as I personally feel I line up more with it than SIBO. On a whole, things for SIBO tend to help me but I personally know I was using a APAP (automated CPAP) in mold. At time, I didn’t know my sleep dysregulation was connected to mold toxcity and I was trying anything for sleep and anxiety. A week after getting my apap, I started getting queasy, anxiety picking up, sleep got worse, feeling sick to stomach. According to info, this just meant the air blowing into stomach was uncovering a IBS problem. Ironic as I never had ANY food intolerances, gut issues, constipation, diaherrea, etc even after living in a moldy home for 10 years. Not even joking. I have every toxic mold present in my body according to the first mycotoxins labs I ran. Again, not joking. That being said, a year later, I found mold hiding behind bathroom tile was causing my health issues which literally I was bedridden with terrible anxiety on top of numerous health issues. And I thought, I wonder if my APAP has mold. I pulled out the humidifier tank. Didn’t see anything. I got a flashlight, and sure enough black mold on the connector tubes. I tried cleaning it but I noticed every time I stuck on the nasal cushion, anxiety increases, my brown would spin, and just mold symptoms increased. I had terrible brain inflammation right out of mold too. I chunked it. Bought a new one. Helped a ton but no matter how much I cleaned new one, I got very anal about it too, I couldn’t keep symptoms down. I would literally be ok. Put on mask, and felt mold symptoms increase. Then the last time I used the humidifier tank, it for really bad. I nvestiagted. The tank was leaking. No mold but my theory is I feel it when dead mycotoxins get watered and are thinking of growing. I finally ditched the humidifier tank and bam. No more issues. 8 hours of water sitting is enough for a sensitive moldy with MCAS to feel it. I never did see mold again in new APAP. I cleaned the tank daily. Never left water sitting. I even have a APAP dryer bc the air drying that most use was enough to bother me and not actually get the tubing, pieces dry. Not using a dryer alone will cause some mold symptoms to flare for me. That being said, I am convinced the APAP was blowing mold into my stomach and caused almost all of my gut symptoms. I suspect its SIFO and not SIBO. I’ve tried finding how to read my OAT test and when you compare mine with SIBO, mine looks alot diff. Almost every mycotoxin on OAT test is high. Bacteria and yeast, actually almost normal. A few markers off but not as bad as the mold markers. The even more interesting part, the ONLY thing that helped me in mold was adrenal supps. The ones I used for high cortisol was holy basil, relora and jujube. First round I used seriphos (form of P.S.) and holy basil. Second time is when I think I began developing MCAS and my body wouldn’t take seriphos. I then switched to holy basil, relora and jujube. The combo didn’t work as well for sleep and anxiety in mold as seriphos but it helped. I still, 2 years later, still take this combo. I actually think treating my adrenals with this combo helped my body hold on so long in mold with such a high level of exposure and very lengthy exposure. I was also exposed as a kid so I know the exposure in old moldy home wasnt only exposure. But it’s when I started having lots of issues. At age 22, my periods flat out stopped for 12 years. A year out or mold and they came back like clock work. I’ve had 7 periods out of mold. I still have a long ways to go but it’s crazy how far I’ve come. I was pulling weeds and gardening yesterday. 2 years ago, I struggled to get out of bed. Taking a bath was pure exhaustive. Just pulling myself out of tub made me go collapse on bed. Barely had enough energy to get my clothes on and walk 20 feet to bed. I get exhausted quickly now, have some major gut issues now, food intolerances, but the progress made just by getting out of mold is mind blowing what mold can do. Anyways, took a hard left hand turn off topic lol. So it would be interesting to see if a CPAP/APAP could be culprit for SIFO. I jusf wonder if holy basil is enough and I need to be patient or something else is needed. Oh and something else I noticed, oregano I do VERY well with. I have another friend who has SIBO confirmed with testing and oregano really does her in. I don’t know if bc I use holy basil, did in mold and out of mold. Or if it’s bc I possibly don’t have SIBO (haven’t tested bc honestly, my root cause to everything has been mold every time) and it’s really just SIFO. I found an environmental doc who has an actual mold treatment center. After so many years of doing this myself, I’ve let him take the lead at this point. He’s got me on supps when I couldn’t. He’s working through food allergies at moment. But some things on testing don’t add up on the food allergies. Anyways. Sorry so long. I have a story to tell I guess lol.
Great article! Interested in trying Argentyn 23 orally. Does it matter if this is taking with food or without? Could it be combined with other supplements (not probiotics)?
Hi Nancy, Argentyn 23 can be with or w/o food and can be combined with any supplements except negatively charged charcoal, clay, chlorella, and zeolite which should be taken away from positively charges supplements (99% of all supplements). Here’s a link to get 15% off Argentyn 23: https://us.fullscript.com/product_cards/83217/redirect?store_slug=mastcell360
Has anyone cleared mold/candida with just taking Sach B? I am taking 10B. twice a day. Is this the max? I am also taking oregano oil 2x a day but I am looking to try just using the Sach B. to spare my good bacteria from damage. Thoughts?
Hi Kelly, what binders you need to take would depend on what mycotoxins you test positive for. We don’t use oregano oil as a mycotoxin binder in our clinic, but we do use sacch B. For proper dosing you will need to discuss with your licensed medical provider who is familiar with your case. To learn more about which binders might be right for you, you can learn more about the testing and binders in this post: https://mastcell360.com/how-to-detox-your-body-from-mold/