
Could You Have SIBO and Histamine Intolerance and/or Mast Cell Activation Syndrome?
When you have issues with Mast Cell Activation Syndrome or Histamine Intolerance, one of the most common root causes can be gut issues.
And these gastrointestinal issues (GI issues) can sneak up on you from anywhere!
You may already be familiar with some autoimmune conditions that affect the gut:
- Irritable Bowel Syndrome (IBS)
- Crohn’s Disease
- Inflammatory Bowel Disease (IBD)
- and even Celiac Disease
But have you heard of SIBO or small intestinal bacterial overgrowth?
In this post, you’ll also learn about:
- What is SIBO?
- Risk factors for getting SIBO
- Symptoms of SIBO
- Testing for SIBO
- How Mold Toxicity affects SIBO
This is part 1 of a 2 part series. I’ll give you a sneak peek at what you’ll see in Part 2 at the end.
This post is for informational and educational purposes only. It is not meant to replace medical advice. Please work with your medical provider on any medical issues. This post is not here to treat, diagnose, or cure any disease or condition, nor is it prescriptive for any person.
What is SIBO?
Small Intestinal Bacterial Overgrowth (SIBO) can be a high number of bacteria living in the small intestine (also called small bowel.)
Even though it’s called small intestinal bacterial overgrowth, it’s more accurate to think of it as bacterial imbalance.
In a healthy gut, you’ll have both good and bad bacteria.
You can also have good and bad fungi, like yeast.
Usually, these microbes keep each other in check.
But when they don’t, the bad can outcompete the good.
That’s why I prefer to think of SIBO as an imbalance.
And when you have this kind of imbalance, it can be rough on your body, especially if you have Mast Cell Activation Syndrome.
I know this firsthand.
I’ve been working on regaining my health for a long time.
And as part of this process, I’ve gone through a lot of trial and error.
That’s why I share my personal stories with you. I want to save you some pain and frustration if I can.
As it happened, in one of my errors of “trial and error”, I got SIBO (and SIFO – you can read the full story in this post.)
SIBO is bad enough on its own.
But SIBO can also contribute to Mast Cell Activation Syndrome. And it can contribute to Histamine Intolerance, too.
Keep reading to learn more about how this happens.
SIBO is all about imbalance of bacteria. But is it always the same type of bacteria? No.
The 3 Types of SIBO
There are different types of bacteria that can overgrow in the small intestine.
Different bacteria species produce different types of gases when they eat their food.
This is why there are different types of SIBO.
Depending on the type, you can get different symptoms.
The 3 main types of SIBO are named after the types of gases produced.
Those gases are:
- Hydrogen
- Methane
- Hydrogen Sulfide
Hydrogen SIBO
Hydrogen SIBO has mostly hydrogen-producing bacteria.
This type of SIBO more often causes diarrhea. But not always.
Methane SIBO
Methane SIBO has mostly methane-producing bacteria.
This type of SIBO more often causes constipation. But again, not always.
Hydrogen Sulfide SIBO
In Hydrogen Sulfide SIBO, your gas can smell like rotten eggs.
It’s VERY noticeable. Like clear the room kind of gas.
This type of SIBO tends to cause diarrhea.
There isn’t as much research on this type of SIBO. And testing for it has just recently become available.
But if you have this type, you will likely have issues with high sulfur foods or hydrogen water.
Of course, you could have a combo of gut imbalances – like SIBO and SIFO.
Related Post: Could SIFO Be Your Root Cause?
That’s why it is important to get more concrete clues about what is going on. Sometimes you can do this with testing.
And that’s why it is important to work with your provider. We’ll get to testing in just a minute.
But first, what leads to these bacterial overgrowths or imbalances? That’s next.
Risk Factors for Small Intestinal Bacterial Overgrowth (SIBO)
There are a number of possible causes behind SIBO.
Keep in mind that you could have multiple causes.
I got SIBO from drinking water from a contaminated source. That’s one way you can get SIBO. But there are others, too.
Here are a few potential risk factors.
Antibiotics
Some examples of antibiotics include:
- metronidazole
- amoxicillin
- ciprofloxacin
- neomycin
Antibiotics can kill off bad bacteria.
But antibiotics can kill off helpful bacteria, too. This can cause imbalances.
High Sugar & Carb Intake
Dietary choices that are high sugar or high carbohydrate, like gluten, can feed harmful bacteria and causes imbalances.
Stress
Stress can affect the movement of food through the intestines.
Undigested food and waste products in the digestive tract create a breeding ground for bacteria.
Mold Toxins
Mold Toxicity is the #1 root cause of Mast Cell Activation Syndrome I see in my practice.
But Mold Toxicity can also cause disruption of the gut, creating imbalances in the microbiome, too.
Low Digestive Enzymes
Low digestive enzymes can result in food not getting properly digested.
Slow passage of food in the digestive tract creates a breeding ground for bacteria.
Low Stomach Acid
Hydrochloric Acid (HCL), called stomach acid, is very important for the digestion of food.
Undigested food and waste products create a breeding ground for bacteria.
This can occur with age or genetics.
Certain Medications
Some medications, can decrease stomach acid production, like protein pump inhibitors (PPIs) for acid reflux:
- Omeprazole (Prilosec)
- Esomeprazole (Nexium)
Loss of GI Motility (gastrointestinal motility)
Loss of GI motility can result in constipation.
Again, slow passage of food and waste products = perfect environment for bacteria to grow
Vagus Nerve Issues
The vagus nerve goes from the neck to the gut.
Any problems with it can affect motility of small & large intestine and stomach emptying.
Certain Surgeries
Surgeries like having your appendix removed or having your colon taken out can slow passage of food and waste products in the digestive tract.
That can create a breeding ground for bacteria.
Age
SIBO risk increases as you get older. This is because you make less stomach acid as you grow older.
Stomach acid breaks down food.
Without enough stomach acid, undigested food can contribute to bacterial imbalance.
Drinking Contaminated Water
Contaminated water can be from:
- accidentally swallowing water from a river or lake
- drinking from an open bottle especially if it’s been uncovered for a few days
- drinking water that hasn’t been treated or tested (ex. well water or water from countries without testing regulations)
- a contaminated water filter or water machine (this is what happened to me)
Clean drinking water is very important!
Now you’ve learned what SIBO is and what can cause it.
Next up take a look at the links between SIBO, Histamine Intolerance, and Mast Cell Activation Syndrome.
SIBO and Histamine Intolerance and Mast Cell Activation Syndrome
Infections are one of the common root causes of mast cell issues.
Small Intestinal Bacterial Overgrowth is one of those possible infections.
Here’s more on how SIBO can contribute to Mast Cell Activation:
- SIBO can cause gut inflammation
- gut inflammation amps up the immune system
- an amped up immune system activates mast cells
- when mast cells are activated, they can release histamine
When mast cells are releasing histamine, that’s adding to your Histamine Load.
If your body is having trouble keeping up with your histamine load, you’ll get Histamine Intolerance.
So by triggering mast cells to release histamine, SIBO can also contribute to Histamine Intolerance.
When I got SIBO, it set me back. I had to get my mast cells calmed down again.
I had to pay extra attention to my histamine load, too.
And I was still dealing with Mold Toxicity, so that made it even harder to kick SIBO.
I’ll tell you more about how Mold Toxicity in just a minute.
But first, you’re probably wondering how to know if you have SIBO.
Next, you’ll learn about symptoms. That’s often your first clue.
Then you’ll learn about testing methods.
Symptoms of Small Intestinal Bacterial Overgrowth (SIBO)
Since SIBO is an issue in the gut, a lot of the symptoms are digestive-related. But not all of them.
Possible symptoms of SIBO:
- bloating
- a distended belly
- intestinal pain or discomfort (cramps)
- gas/flatulence
- heartburn
- acid reflux
- belching
- diarrhea
- constipation
- low energy
- weight loss
Malabsorption can also happen with SIBO.
This is where your body has problems absorbing nutrients like iron, vitamin B12, and vitamin D.
This can lead to malnutrition, vitamin deficiencies and anemia, too.
Bone loss – osteoporosis or osteopenia – can be related to SIBO, too.
This is because with gut inflammation from SIBO, you might get mineral loss.
But sometimes SIBO doesn’t cause any symptoms at all.
Or, the symptoms may be misinterpreted.
So, other than symptoms, how can you know for sure which type of SIBO you have?
Or, how do you know if you have SIBO at all? We’ll go over testing options next.
Testing for Small Intestinal Bacterial Overgrowth (SIBO)
Another reminder: This post is for informational and educational purposes only. It is not meant to replace medical advice. Please work with your medical provider on any medical issues. This post is not here to treat, diagnose, or cure any disease or condition, nor is it prescriptive for any person.
There are a few tests that can help determine if you have SIBO.
You’ll want to talk with your healthcare practitioner if you think you have SIBO.
Your healthcare practitioner can help you know if one of these tests might be right for you.
Here are a few of the common tests.
1. Breath Testing
Testing for SIBO is usually done using Breath Testing.
Remember, there are 3 types of SIBO:
- Hydrogen SIBO
- Methane SIBO
- and Hydrogen Sulfide SIBO
Different tests will look for each kind of gas.
For example, the hydrogen breath test looks for Hydrogen SIBO.
But to prepare for these tests, you have to drink a type of sugar (like lactulose syrup) that triggers more bacterial growth and activity.
It’s very important to follow the test prep instructions exactly as they are written.
And it’s important to do that with your medical practitioner’s guidance.
Pros:
- widely available
- non-invasive
Cons:
- you must drink a sugary drink to trigger bacterial activity
- 50% false positive rate
2. Small Intestine Aspirate and Fluid Culture
Aspirate means something is being suctioned out of your body. In this case, it would be intestinal fluids.
This type of testing requires a doctor to pass a tube down your throat to reach the small intestine.
That’s how they collect a fluid sample to test for bacteria growth.
Pros:
- considered the gold standard by doctors
Cons:.
- invasive
- requires prep and anesthesia which can trigger mast cell activation
- can miss SIBO 40% of the time
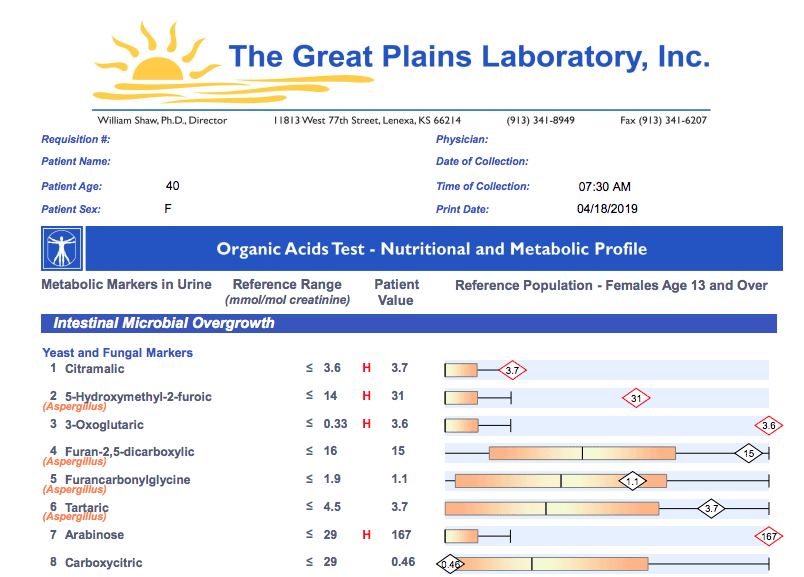
3. Organic Acid Testing
There is a test called the Microbial Organic Acids Test.
It tests organic acids that are produced by the bacteria you have.
It has some good markers for both bacteria and gut fungal species.
Great Plains Labs offers a great Microbial Organic Acids Test (mOAT).
Pros:
- can order this directly without needing a provider
Cons:
- can’t tell where the bacteria or fungi are located – could be overgrown in either the large or small intestine.
- gives indirect information – not specific regarding SIBO
But, at least you’ll know whether the levels are high. That can be helpful in figuring out what’s going on.
So, the mOAT may be a good test to start with.
Here is a sample of the Great Plains Labs Microbial Organic Acids Test:
4. Mold Toxins Testing
If you keep trying gut or SIBO protocols… and you aren’t getting better… then it’s usually time to check for mold toxins.
Mold can keep you from getting rid of SIBO.
In fact, mold toxins are one of the BIGGEST reasons I see SIBO protocols fail for people over and over.
This is because mold toxins get dumped into the gut.
Then no matter what you do to heal your gut, the mold toxins cause more damage.
And mold toxicity has truly become a hidden epidemic.
For about 99% of the people I see in the Mast Cell 360 clinic, Mold Toxicity is an underlying condition.
Urine testing can let you know what level of mold toxins are being eliminated from the body.
But there isn’t one panel that covers all the mold markers.
So, I use 2. They complement each other.
1. RealTime Mycotoxin Panel
Not available in New York, New Jersey, or Rhode Island
>>> Order the RealTime Mycotoxin Panel here
2. Great Plains Mycotoxin Test
>>> In the US use this link to order the Great Plains Mycotoxin Test
>>> In Canada use this link to order the Great Plains Mycotoxin Test
Be sure to read about these tests and get the provocation information here.
But why is mold testing important if you think you have SIBO? I’ll go over that next.
Mold Toxins and Small Intestinal Bacterial Overgrowth (SIBO)
Mold Toxins can worsen SIBO. They do this by continually disrupting the gut bacteria.
This is because mold toxins get dumped into the gut. And then they can cause a lot of problems.
Mold toxins affect your entire immune system.
In regard to SIBO, mold toxins affect the body’s ability to keep bacteria levels in the gut in check.
And mold toxins increase mast cell activation at the same time.
When this happens, normal bacteria in the gut can overgrow.
Or bad bacteria can grow out of control.
And mold toxins can contribute to leaky gut. That’s where you get intestinal permeability.
That just means all kinds of stuff that should not be passing through the walls of your intestine are leaking through. Including bacteria.
I have seen people try to get rid of SIBO for years with little luck.
It was most often because the mold toxins weren’t addressed first.
If you DO have mold toxins, address those first.
If you find out you do have mold toxicity, then you’ll want to address it slowly.
But, here’s the good news!
SIBO is usually much easier to address once mold toxins are out of your system. You can read some of the basics of addressing mold toxins in these posts.
- Mycotoxins and Mold: One of the Biggest Root Triggers for Mast Cell Activation & Histamine Intolerance
- How to Detox Your Body From Mold Gently
- Addressing Mold Toxicity
So, if you can’t get rid of SIBO, check for mold and address it first.
If you don’t have Mold Toxicity or you’ve dealt with that factor, then what can you do for SIBO?
Next Steps for SIBO and Histamine Intolerance
That’s what you’ll learn in Part 2 on SIBO, especially if you have SIBO and Histamine Intolerance and/or Mast Cell Activation Syndrome.
I’ll share with you my gentle protocol that I use with my private clients.
You’ll learn more about
- why some food intolerances and food sensitivities can be the result of SIBO (you’ll particularly want to check out this article if you have Histamine Intolerance)
- how high histamine foods that lead to build up of histamine and high histamine levels can really affect your gut health
And you’ll learn how to support your dietary needs with options like:
- low histamine diet
- low fodmap diet
- elemental diet
- foods that will support gut health
You’ll also read about:
- probiotics
- gut health supplements
- supplements which can help support histamine intolerance (like DAO diamine oxidase)
- supplements which can help support the mast cells (like quercetin)
Related Article: Can Paraprobiotics Support Mast Cells?
You’ll also learn how lifestyle adaptations can help. These include supports like:
- nervous system support
- additional tips on how to support GI motility
Do you think you are dealing with SIBO and Histamine Intolerance and/or Mast Cell Activation Syndrome?
More From Mast Cell 360
- Part 2: SIBO Diet, Lifestyle Changes, and Supplements for MCAS and HIT
- Frequently Asked Questions: The Gut, SIBO, Mast Cell Activation Syndrome, and Histamine Intolerance
- Lyme, SIBO, Candida, EBV in Mold Toxicity – Why won’t they go away? What do you do to get rid of them?
- What is SIFO? Is it a Mast Cell Trigger like Mold?
Some links in this website are affiliate links, which means Mast Cell 360 may make a very small commission if you purchase through the link. It never costs you any more to purchase through the links, and we try to find the best deals we can. We only recommend products that we love and use personally or use in the Mast Cell 360 practice. Any commissions help support the newsletter, website, and ongoing research so Mast Cell 360 can continue to offer you free tips, recipes, and info. Thank you for your support!
References
Belapurkar, P., Goyal, P., & Tiwari-Barua, P. (2014). Immunomodulatory effects of triphala and its individual constituents: a review. Indian journal of pharmaceutical sciences, 76(6), 467–475.
Borlinghaus, J., Albrecht, F., Gruhlke, M. C., Nwachukwu, I. D., & Slusarenko, A. J. (2014). Allicin: chemistry and biological properties. Molecules (Basel, Switzerland), 19(8), 12591–12618. https://doi.org/10.3390/molecules190812591
Brown, K., Scott-Hoy, B., & Jennings, L. W. (2016). Response of irritable bowel syndrome with constipation patients administered a combined quebracho/conker tree/M. balsamea Willd extract. World journal of gastrointestinal pharmacology and therapeutics, 7(3), 463–468. https://doi.org/10.4292/wjgpt.v7.i3.463
Bures, J., Cyrany, J., Kohoutova, D., Förstl, M., Rejchrt, S., Kvetina, J., Vorisek, V., & Kopacova, M. (2010). Small intestinal bacterial overgrowth syndrome. World journal of gastroenterology, 16(24), 2978–2990. https://doi.org/10.3748/wjg.v16.i24.2978
d’Alessio, P. A., Ostan, R., Bisson, J. F., Schulzke, J. D., Ursini, M. V., & Béné, M. C. (2013). Oral administration of d-limonene controls inflammation in rat colitis and displays anti-inflammatory properties as diet supplementation in humans. Life sciences, 92(24-26), 1151–1156. https://doi.org/10.1016/j.lfs.2013.04.013
Ducrotté, P., Sawant, P., & Jayanthi, V. (2012). Clinical trial: Lactobacillus plantarum 299v (DSM 9843) improves symptoms of irritable bowel syndrome. World journal of gastroenterology, 18(30), 4012–4018. https://doi.org/10.3748/wjg.v18.i30.4012
Ghayur, M. N., & Gilani, A. H. (2005). Pharmacological basis for the medicinal use of ginger in gastrointestinal disorders. Digestive diseases and sciences, 50(10), 1889–1897. https://doi.org/10.1007/s10620-005-2957-2
Giannini, E. G., Mansi, C., Dulbecco, P., & Savarino, V. (2006). Role of partially hydrolyzed guar gum in the treatment of irritable bowel syndrome. Nutrition (Burbank, Los Angeles County, Calif.), 22(3), 334–342. https://doi.org/10.1016/j.nut.2005.10.003
Goulet, O., & Joly, F. (2010). Microbiote intestinal dans le syndrome du grêle court [Intestinal microbiota in short bowel syndrome]. Gastroenterologie clinique et biologique, 34 Suppl 1, S37–S43. https://doi.org/10.1016/S0399-8320(10)70019-1
Grundy, D., Hutson, D., & Scratcherd, T. (1986). A permissive role for the vagus nerves in the genesis of antro-antral reflexes in the anaesthetized ferret. The Journal of physiology, 381, 377–384. https://doi.org/10.1113/jphysiol.1986.sp016332
Hirota, R., Roger, N. N., Nakamura, H., Song, H. S., Sawamura, M., & Suganuma, N. (2010). Anti-inflammatory effects of limonene from yuzu (Citrus junos Tanaka) essential oil on eosinophils. Journal of food science, 75(3), H87–H92. https://doi.org/10.1111/j.1750-3841.2010.01541.x
Horwitz, R. J. (2018). The Allergic Patient. Integrative Medicine, 300–309.e2. https://doi.org/10.1016/b978-0-323-35868-2.00030-x
Hu, M. L., Rayner, C. K., Wu, K. L., Chuah, S. K., Tai, W. C., Chou, Y. P., Chiu, Y. C., Chiu, K. W., & Hu, T. H. (2011). Effect of ginger on gastric motility and symptoms of functional dyspepsia. World journal of gastroenterology, 17(1), 105–110. https://doi.org/10.3748/wjg.v17.i1.105
Jerobin, J., Makwana, P., Suresh Kumar, R. S., Sundaramoorthy, R., Mukherjee, A., & Chandrasekaran, N. (2015). Antibacterial activity of neem nanoemulsion and its toxicity assessment on human lymphocytes in vitro. International journal of nanomedicine, 10 Suppl 1(Suppl 1), 77–86. https://doi.org/10.2147/IJN.S79983
Kinross, J.M., Darzi, A.W. & Nicholson, J.K. (2011). Gut microbiome-host interactions in health and disease. Genome Medicine. 3, 14. https://doi.org/10.1186/gm228
Kritas, S. K., Gallenga, C. E., D Ovidio, C., Ronconi, G., Caraffa, A. l., Toniato, E., Lauritano, D., & Conti, P. (2018). Impact of mold on mast cell-cytokine immune response. Journal of biological regulators and homeostatic agents, 32(4), 763–768.
Lin, E. C. & Massey, B. T. Scintigraphy Demonstrates High Rate of False-positive Results From Glucose Breath Tests for Small Bowel Bacterial Overgrowth. Clinical Gastroenterology and Hepatology 14, 203–208 (2016).
Lo, W. K., & Chan, W. W. (2013). Proton pump inhibitor use and the risk of small intestinal bacterial overgrowth: a meta-analysis. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association, 11(5), 483–490. https://doi.org/10.1016/j.cgh.2012.12.011
Mailing, L. (2019, November 12). What the latest research reveals about SIBO. Lucy Mailing, PhD. https://www.lucymailing.com/what-the-latest-research-reveals-about-sibo/
Mailing, L. (2020, July 5). All about SIBO: Small Intestinal Bacterial Overgrowth. Lucy Mailing, PhD. https://www.lucymailing.com/all-about-sibo-small-intestinal-bacterial-overgrowth/
Malbert C. H. (2005). The ileocolonic sphincter. Neurogastroenterology and motility : the official journal of the European Gastrointestinal Motility Society, 17 Suppl 1, 41–49. https://doi.org/10.1111/j.1365-2982.2005.00657.x
Mayo Clinic. (2022, January 6). Small intestinal bacterial overgrowth (SIBO) – Diagnosis and treatment – Mayo Clinic. Retrieved April 30, 2022, from https://www.mayoclinic.org/diseases-conditions/small-intestinal-bacterial-overgrowth/diagnosis-treatment/drc-20370172
Mayo Clinic. (2022, April 11). Charcoal, Activated (Oral Route). Retrieved April 30, 2022, from https://www.mayoclinic.org/drugs-supplements/charcoal-activated-oral-route/description/drg-20070087
Nathan, N. (2018). Toxic: Heal your body from Mold Toxicity, lyme disease, multiple chemical sensitivities, and chronic environmental illness. Victory Belt Publishing.
Pereira, A. P., et al. (2007). Phenolic compounds and antimicrobial activity of olive (Olea europaea L. Cv. Cobrançosa) leaves. Molecules (Basel, Switzerland), 12(5), 1153–1162. https://doi.org/10.3390/12051153
Pimentel, M., et al. (2004). A 14-day elemental diet is highly effective in normalizing the lactulose breath test. Digestive diseases and sciences, 49(1), 73–77. https://doi.org/10.1023/b:ddas.0000011605.43979.e1
Rao, S., Tan, G., Abdulla, H., Yu, S., Larion, S., & Leelasinjaroen, P. (2018). Does colectomy predispose to small intestinal bacterial (SIBO) and fungal overgrowth (SIFO)?. Clinical and translational gastroenterology, 9(4), 146. https://doi.org/10.1038/s41424-018-0011-x
Ratnaseelan, A. M., Tsilioni, I., & Theoharides, T. C. (2018). Effects of Mycotoxins on Neuropsychiatric Symptoms and Immune Processes. Clinical therapeutics, 40(6), 903–917. https://doi.org/10.1016/j.clinthera.2018.05.004
Rezaie, A., et al. (2017). Hydrogen and Methane-Based Breath Testing in Gastrointestinal Disorders: The North American Consensus. The American journal of gastroenterology, 112(5), 775–784. https://doi.org/10.1038/ajg.2017.46
Small intestinal bacterial overgrowth (SIBO) – Symptoms and causes. (2020, February 28). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/small-intestinal-bacterial-overgrowth/symptoms-causes/syc-20370168
Subapriya, R., & Nagini, S. (2005). Medicinal properties of neem leaves: a review. Current medicinal chemistry. Anti-cancer agents, 5(2). https://doi.org/10.2174/1568011053174828
Takahashi T. (2012). Mechanism of interdigestive migrating motor complex. Journal of neurogastroenterology and motility, 18(3), 246–257. https://doi.org/10.5056/jnm.2012.18.3.246
Tamhane, M. D., Thorat, S. P., Rege, N. N., & Dahanukar, S. A. (1997). Effect of oral administration of Terminalia chebula on gastric emptying: an experimental study. Journal of postgraduate medicine, 43(1), 12–13.




Add A Comment