
Do You Have One or Both? Histamine Intolerance vs MCAS (Mast Cell Activation Syndrome)
Are you trying to put together the pieces of your health issues? Maybe you’ve tried a low histamine diet?
Do you suspect you have Histamine Intolerance or Mast Cell Activation Syndrome?
Understanding these conditions can feel like trying to put together a puzzle without knowing what the picture is! But I want to help you with that.
For many people, Histamine Intolerance and Mast Cell Activation Syndrome (MCAS) go hand-in-hand.
In fact, they can have similar symptoms.
But they are two separate conditions.
You can have both or just one.
It’s important to know the difference so you can address them properly.
Keep reading to learn about:
- Histamine Intolerance vs Mast Cell Activation Syndrome
- What is Mast Cell Activation Syndrome?
- What is Histamine Intolerance?
- How Mast Cell Activation and Histamine Intolerance Feed Into One Another
- Mast Cell Activation Syndrome without Histamine Intolerance
- Histamine Intolerance without Mast Cell Activation Syndrome
- Supplements for Histamine Intolerance vs MCAS
It’s important you know that this blog post is for informational and educational purposes. It’s not meant to treat any health condition or to be prescriptive for anyone. If you have any medical condition, it is critical you work under the care and guidance of a licensed medical provider.
Histamine Intolerance vs Mast Cell Activation Syndrome
Mast Cell Activation Syndrome and Histamine Intolerance share many symptoms. And they may look like other conditions, too.
Always be sure to talk with your licensed medical provider to rule out other medical conditions. That’s very important, and I can’t stress that enough.
Just because your symptoms look like Histamine Intolerance or Mast Cell Activation Syndrome, that doesn’t mean they are necessarily related.
For example, heart palpitations may be a symptom of Mast Cell Activation Syndrome.
But heart palpitations may be a sign of a serious cardiovascular condition, too.
That’s just one example.
But you can see why it’s so important to look at all possibilities with your medical provider to rule out serious medical conditions.
But if you rule out other serious conditions, and are considering Histamine Intolerance and Mast Cell Activation Syndrome, keep reading to learn more.
Let’s start by looking at what each of these conditions are.
What Is Mast Cell Activation Syndrome?
Mast Cell Activation Syndrome (MCAS) is when your mast cells become overly responsive.
It helps to understand MCAS by understanding mast cells and the role they play in your body.
Mast cells are a part of your immune system. They are one of your body’s first lines of defense against invaders.
Read more: What Are Mast Cells?
Here’s a comparison which may help you understand mast cells and Mast Cell Activation Syndrome more easily.
Your mast cells are the guards of the castle. The castle is your body.
When intruders like viruses, bacteria, mold, toxins, and allergens come around, the guards take up arms.
They start attacking those intruders to protect you.
Mast cells are very important to keeping you healthy and safe.
But here’s what happens with Mast Cell Activation Syndrome.
The guards have been attacked for months and months on end. They don’t get to take a break or rest.
When they can’t take a break, they get dysregulated.
And this means they don’t have a clear idea of who the enemy is anymore.
It’s kind of like if you don’t sleep for months and your brain goes wonky.
You can’t tell what’s real anymore.
The mast cells can’t tell what friend or foe is, and instead they just started fighting everything… or at least what can feel like everything.
This can result in food, supplement, and chemical sensitivities.
Another thing that can happen is the mast cell guards might be getting the wrong messages from the lookout tower.
The lookout tower is what we’ll call the mast cell receptors.
Mast cell receptors are part of cell signaling – how cells talk with one another and receive information about their environment.
Communication between the cells and molecules outside of the cells happens in cell signaling through the receptors.
Sometimes the receptors get overly sensitive. This means they’re sending the wrong messages.
So, the guards may have gotten the message from the lookout tower to attack the wrong thing.
This can often be the case when mold is involved. Mold Toxicity isn’t the only thing that can throw off the mast cell responses.
Mold is the most common one I see in the Mast Cell 360 practice, though.
Lyme and other tickborne infections are other big triggers as well.
But 99% of my clients have mold toxicity as a root cause of Mast Cell Activation Syndrome.
Before we get more into that, let’s look at some of the symptoms of MCAS.
Symptoms of Mast Cell Activation Syndrome
Here are some clues that you may want to look into Mast Cell Activation Syndrome for yourself.
Do you have:
- Symptoms that you or your medical provider can’t explain?
- Many kinds of symptoms?
- Inflammatory symptoms in at least 2 or more systems in your body (like your skin and gut, or your brain and lungs)?
This may be mast cell related.
Mast cells are in almost every part of your body. That’s why so many different symptoms and conditions can be mast cell related.
Some of these symptoms are the same as the symptoms of Histamine Intolerance, too.
Common symptoms of both Mast Cell Activation Syndrome and Histamine Intolerance include:
- Anxiety
- Depression
- Asthma or other issues with shortness of breath
- Fatigue
- Gut and gastrointestinal issues like diarrhea or constipation
- Headaches
- Inflammation/swelling
- Insomnia
- Sinus issues like congestion or runny nose
- Skin issues like hives, rashes, or flushing
But there are many, many more symptoms and conditions related to Mast Cell Activation Syndrome.
And Mast Cell Activation Syndrome is usually much more severe than if someone just has Histamine Intolerance.
Because there are so many possible symptoms, you can take a look at this symptoms survey to see how many may apply to you.
But consider just a few of the following for now. Are you dealing with any of these in addition to the symptoms above?
Unique symptoms that may indicate you are dealing with Mast Cell Activation Syndrome:
- Anaphylaxis
- Autoimmune disorders
- Brain fog
- Chemical sensitivities
- Chronic infections
- Difficulty healing
- History of toxic mold exposures
- History of Lyme or other tickborne infections
- Sensitivities to light or sound
If any of these sound familiar, you may want to consider Mast Cell Activation Syndrome.
Like you read, mast cells perform a normal job of keeping you healthy. But they can go haywire.
There are a few major ways I see this happen. I call these root causes.
Now that we’ve talked about what MCAS is, let’s look at some root causes next.
Root Causes of MCAS
There are many things that can contribute to the mast cell dysregulation in Mast Cell Activation Syndrome.
Some of these root causes can include:
- Mold Toxicity
- Mold Colonization
- Nervous system dysregulation
- Food triggers like histamine, lectins, and oxalates
- Infections like Lyme and Epstein Barre
- Hormonal imbalances
- Chronic stress and trauma (including childhood trauma)
Those are a few of the big picture things that can lead to overly responsive or “haywire” mast cells.
To understand how mast cells go haywire, first look at how a normal mast cell response should work.
Your mast cells have over 200 different types of receptors. Receptors are the lookout tower you read about earlier.
They respond to everything that happens outside your body and everything that happens inside your body.
One way they respond is by releasing chemicals called mast cell mediators.
You may already be familiar with one of these mast cell mediators: histamine.
If you aren’t familiar with it, you’ll read more about it coming up.
Some other mediators you may have heard of include cytokines, tryptase, and prostaglandins.
These mediators play important roles in your body including:
- Fighting infections
- Removing toxins
- Repairing injuries
- Signaling pain
- Supporting good sleep patterns
- Balancing hormones
- And more
Normally, your mast cells launch a response to help keep you healthy.
For example, you may get histamine release to induce inflammation. Inflammation may help get more blood to an injured area to help with healing.
Once the threat has been dealt with, mast cells should stabilize again.
They should quit releasing the mediators.
But when you’re dealing with root causes that make the mast cells become dysregulated, the mast cells don’t stabilize.
They can continue to release inflammatory mediators… like histamine.
If the mast cells stay dysregulated, they can release more histamine than your body can break down.
On top of that, a lot of MCAS triggers can affect your ability to break down histamine, too.
That’s one reason why you’ll often see Mast Cell Activation and Histamine Intolerance together.
So, let’s look more at Histamine Intolerance next.
What Is Histamine Intolerance?
Histamine Intolerance is when your body can’t handle the levels of histamine built up in your body.
The amount of histamine your body can handle is sometimes called your histamine load.
You can add to your histamine load by eating high histamine foods.
Or histamine liberating foods. That means some foods may not contain a lot of histamine, but they can trigger histamine release.
That’s why I list things like some citrus fruits as “high histamine” to keep things simple.
And some foods and drinks, like alcoholic beverages and black teas, may affect histamine in yet another way. They can weaken the production of the enzymes your body makes to break down histamine. I list those as “high histamine,” too.
My low histamine foods list can help you find which foods are lower and higher histamine.
And earlier you read about another way you can add to your histamine load – your body makes histamine.
You just read that histamine is one of the mediators that gets released by your mast cells.
And that mediators like histamine play a role in normal immune responses.
That means if you get a runny nose or itchy eyes occasionally that might just be because you were exposed to something your body didn’t like… like an allergen.
And your body is trying to get rid of it.
This is natural. It doesn’t mean you have Histamine Intolerance.
Again, Histamine Intolerance is when you have TOO MUCH histamine in your body.
See, histamine has to get broken down in your body by enzymes.
The enzyme activity has to be able to keep up with the amount of histamine in your body.
If it can’t, histamine will cause problems for you.
It may help you understand Histamine Intolerance by comparing it to a kitchen sink.
The sink is your body. The water that flows from the faucet is histamine. And the drain is the enzymes that break down the histamine.
If your drain is open all the way and working well, all the water that flows from the faucet goes right down the drain.
No problem.
But what if that drain is clogged?
The drain can’t get rid of the water as fast as new water is flowing in.
Now water is building up in the sink.
Before too long, your sink is so full that water spills over the edge and all over your floor. Now you’ve got problems.
That’s like histamine.
If your body isn’t getting rid of it, histamine builds up and causes problems.
While histamine plays an important role in the body’s regular functions, too much histamine can be bad.
Why does histamine build up? Keep reading to learn more.
Why Does Histamine Build Up in Your Body?
Now you know what contributes to your histamine load. But what leads to Histamine Intolerance?
For some people, their body can keep up with their histamine load, both from foods and the body’s production.
But that’s not the case for everyone. For some people, histamine builds up in the body.
There are a number of different factors that can cause histamine to build up.
One of the biggest ones is that your body isn’t making enough of the enzymes that break histamine down.
Here’s why that may be happening.
Histamine Degrading Enzymes
Your body may not be making enough histamine degrading enzymes.
The 2 main enzymes that break down histamine are DAO and HNMT. There are others, but these are the 2 we’ll focus on here.
DAO (diamine oxidase) primarily breaks down histamine in the gut.
HNMT (Histamine N-methyltransferase) breaks down histamine outside the gut.
Did you know? Histamine that starts out in the gut can overflow and enter the bloodstream?
Your body may not be making enough DAO or HNMT. Or it may not be making enough of the compounds DAO or HNMT need to be activated.
This may be due to factors like the following:
Gut Inflammation
Your body can have trouble making DAO if you have gut inflammation.
Low Nutrients Like Zinc, B6, Copper, and Vitamin C
DAO needs a variety of nutrients to work. Without these DAO won’t activate and break down histamine like it should.
But did you know supplements can be part of the histamine problem? For example, vitamin C is often fermented! Which means higher histamine. I talk about how to find a low histamine vitamin C here.
And all the supplements I recommend on the blog are low histamine.
Methylation Issues
Methylation is a process that produces HNMT (the histamine degrading enzyme) and a compound called SAMe (S-Adenosyl-L-Methionine).
SAMe is needed to activate the enzyme HNMT that you read about earlier.
If your methylation process is messed up, you might not produce enough SAMe or HNMT.
I don’t recommend supplementing with SAMe except in rare cases.
And in the MC360® Method, we normally don’t introduce methylation supports for sensitive people until the other detox pathways are better supported.
But if you are at the point where you are considering methylation supports, here are a couple ideas to consider.
The methylation cycle is complex. Many nutrients are needed for methylation. These are just 2 ideas.
Zinc picolinate is one of the cofactors needed. It’s a gentler starting supplement if you have any supplement sensitivities.
If you aren’t sensitive and can handle a combo product, you could also consider Homocysteine Factors, a blend of vitamins and nutrients.
What all this comes down to is that if you don’t have enough of these histamine degrading enzymes to keep up with the histamine you are making or consuming, your sink overflows – and you get Histamine Intolerance.
Your body says, “We aren’t going to tolerate any more!” So, you start having reactions.
It’s your body’s way of saying stop or slow down so I can deal with this!
Now that you know more about these two conditions, let’s look a little closer at having one or both, and how they can feed into each other.
How Mast Cell Activation Syndrome and Histamine Intolerance Feed Into One Another
Let’s start by looking at why Mast Cell Activation Syndrome and Histamine Intolerance may be seen together.
When you read about Mast Cell Activation Syndrome (MCAS), you learned that mast cells can release histamine.
And with MCAS, your mast cells are overly response.
That means your mast cells are releasing histamine. A lot of it!
This can become a self-feeding cycle.
Here’s how:
- Histamine can trigger mast cells
- When triggered, mast cells release more histamine
- More histamine causes more histamine release
It’s like a forest fire that starts with a little spark and slowly burns out of control.
This over release of histamine can contribute to Histamine Intolerance.
You might be producing so much histamine that your body can’t keep up.
But mast cell activation doesn’t always mean Histamine Intolerance.
Let’s look at how you can have Mast Cell Activation Syndrome without Histamine Intolerance, next.
Mast Cell Activation Syndrome Without Histamine Intolerance
When you learned about Histamine Intolerance, you learned that this happens when your body can’t keep up with your histamine load.
And you just read how mast cells release histamine and how this cycle can feed into itself.
And you read that all this histamine may be too much for your body to keep up.
But, if your body CAN keep up with your histamine load, you might only have Mast Cell Acitvation Syndrome.
Again, Mast Cell Activation Syndrome is when you have overly reactive mast cells.
This might be from any of those root causes you read about earlier… like mold.
Here are some clues that you might be dealing with Mast Cell Activation Syndrome.
Reaction Time
Reaction time can be a clue you have Mast Cell Activation Syndrome (MCAS).
With MCAS, you may experience reactions within 30 minutes of coming into contact with a trigger.
If your mast cells are overly reactive, you might be sensitive to:
- Certain foods
- Supplements
- Medications
- Skincare products or fragrance
Mast cell reactions can happen within seconds to minutes after exposure to a trigger.
This is a classic sign.
There can also be delayed reactions from hours to days later as well with MCAS. So, you can’t rule out MCAS if you have delayed reactions.
But if you react right away, consider mast cell involvement.
One example would be if you react when you smell a food.
Or do your reactions to foods start before you even finish your meal? If so, that’s more likely a mast cell response vs a histamine response.
Symptoms in 2 or More Body Systems
Another clue for Mast Cell Activation Syndrome is having symptoms in 2 or more of the systems of your body.
For example, do you have gut issues like chronic diarrhea, and do you also have chronic skin conditions like hives?
That’s two different systems: your digestive system and what’s called your integumentary system.
Another example would be if you have migraines (nervous system) and asthma (respiratory). That’s two different systems of the body.
So, that’s how you can have Mast Cell Activation without Histamine Intolerance.
Next, let’s look at how what it means if you just have Histamine Intolerance without having MCAS.
Histamine Intolerance Without Mast Cell Activation Syndrome
If your body doesn’t have overly reactive mast cells, you may just be dealing with Histamine Intolerance.
In these instances, your histamine overload is likely mostly a result of the foods you eat.
Think about this:
- Are you able to walk down the aisle of laundry detergent without any issues?
- Do you feel worlds better if you stick with low histamine foods?
- Do high histamine foods seem to be your only sensitivity?
If you answered yes to those questions, you may just have Histamine Intolerance.
And unlike mast cell reactions that can show up almost immediately, histamine reactions usually need at least 30 minutes to set up.
This is because your body needs a chance to absorb the histamine from the foods.
Even the act of digestion will create histamine.
And histamine reactions can happen hours or even up to a couple of days later.
So, the reaction will not be immediate if it’s just Histamine Intolerance.
If your symptoms get a lot better with a low histamine diet, Histamine Intolerance may be what you need to explore further.
Those who have Mast Cell Activation Syndrome tend to have sensitivities beyond just histamine foods, though.
So, if your mast cells are not overly reactive in general, you may be able to just do a few supplements like DAO, that help with histamine breakdown.
At this point, if you think you have either Mast Cell Activation, Histamine Intolerance or both, you’re probably wondering what can be done.
Many of the things you do to support Histamine Intolerance will also support Mast Cell Activation Syndrome.
But a couple are different. Let’s look at both now.
Supplements for Histamine Intolerance vs MCAS
Here are some things you can talk to your practitioner about that may help if you have Mast Cell Activation Syndrome or Histamine Intolerance.
DAO
For histamine you get from foods, you might consider supplementing DAO (diamine oxidase).
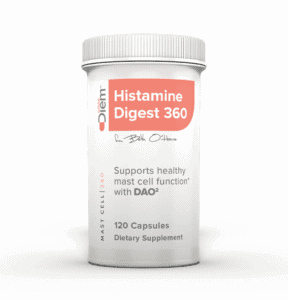
I even created a custom DAO specifically for those in our Mast Cell 360® community.
It doesn’t have all the fillers that some formulas have.
Fillers can sometimes be made from high histamine or mast cell-triggering ingredients.
And this formula has 1mg of vitamin B6 per capsule. This is a very tiny amount of B6.
Remember how you read earlier that B6 is an important co-factor for DAO? You need enough B6 to activate DAO.
I find many of my clients are low in B6, though.
So, when they take other DAO supplements, they often don’t work for them.
That’s why there is just enough B6 in this custom Histamine Digest 360 DAO formula to activate it, so it works.
Quercetin
Quercetin may help with both histamine and mast cell support.
Many herbal antihistamines include this ingredient.
Quercetin has been shown in studies to:
- Have mast cell supporting properties
- Improve respiratory symptoms, like asthma
- Inhibit tryptase, an inflammatory mast cell mediator
- Inhibit the enzyme HDC, which converts the amino acid histidine (found in foods) to histamine
This Alpha-glycosyl Isoquercitrin is one of my favorites!
Learn more: Health Benefits of Quercetin
Perilla Seed Extract
Perilla seed extract can be good for histamine intolerance.
It’s one type of natural antihistamines. It may also help with Mast Cell Activation Syndrome.
Research has shown perilla seed to:
- Reduce histamine
- Reduce the mast cell cytokine TNF-a
- Have anti-inflammatory properties
- Reduce allergic skin reactions
- Improve respiratory symptoms
This Perilla Seed Extract is the one I prefer.
Read more: Perilla Seed Extract
DAO, quercetin, and perilla seed extract are just a few of the supplements you might consider.
To learn more about these and other supplement recommendations, check out my Top 8 Mast Cell Supporting Supplements Master Class.
In addition to supplements, there are other things you can consider, too. Keep reading to learn about those.
Low Histamine Diet
Before you change your diet on your own, please make sure you’re working with a healthcare practitioner who can help you with this. Never limit foods unnecessarily, and always have a licensed medical provider who is supervising your case.
Reducing the amount of high histamine foods you eat will definitely help lower your histamine load.
Learn more: Low Histamine Diet Plan
But be very careful about some of the food lists you see online.
Some list any food that anyone has had a reaction to for any reason. That’s not very helpful.
It can mean you’ll be missing out on more options for nutritional variety.
Other lists leave out the histamine liberators.
And many list high histamine foods as ok!
I’ve found that, unfortunately, most of the low histamine lists online have at least 1 or more of these mistakes.
Also, if you’re going to eat low histamine, always be sure to think in terms of replacing rather than removing.
I really want to emphasize this.
For example, spinach is high histamine. But in place of spinach in salads, you can try arugula instead.
Instead of strawberries, you can try cherries instead.
Instead of high-histamine aged beef, try beef or bison that hasn’t been aged.
You can find some great low histamine options from companies like Northstar Bison.

>>> Use coupon code MASTCELL360 for 10% off all of their low histamine meats!
And for even more options, check out: The Best Low Histamine Meat and Seafood
Nervous System Support
Supporting your nervous system can help with both Mast Cell Activation Syndrome and Histamine Intolerance.
Read more: Nervous System Balance is Essential
In the Mast Cell 360® practice, I’ve seen clients have tremendous breakthroughs once they address the nervous system support piece.
You read that dysregulated mast cell signaling can result in over reactive mast cells. Getting those signals calmed down can help in a number of ways.
It can start giving your “mast cell guards” a rest.
Working toward a parasympathetic state (rest, heal, digest) is so important.
Nervous system support can help you start to feel like you aren’t in a constant state of needing to defend or attack whatever comes your way.
Once your mast cells aren’t constantly feeling triggered, you can get some relief from your mast cell symptoms.
And because your mast cells aren’t activating and releasing histamine, you’ll get some relief from your histamine related symptoms, too.
To learn more about nervous system support and put together a personalized plan, try my Mast Cell Nervous System Reboot Course.
Address Mold Toxicity
Mold does a lot of damage in the body.
Earlier, you learned mold can contribute to Mast Cell Activation Syndrome.
Mold Toxicity can cause severe nervous system and immune system dysregulation.
When your nervous system and your immune system aren’t functioning properly, the chances for mast cell dysregulation are much higher.
Mold can also cause issues in the gut.
And gut issues can lead to nervous system and immune system dysregulation, too.
And like you read, gut inflammation can affect your production of DAO, the histamine degrading enzyme.
I put together an entire course that walks you through what mold is, how to test for it, supports, detox pathways, binders, and the steps we take in the clinic.
You can learn all about mold in my MC360™ Precision Mold Master Class.
The body is connected in so many ways. It’s truly amazing.
But all that interconnectedness can be a domino effect for your health.
That’s why we look at the whole picture.
I hope this overview helped you understand Histamine Intolerance vs MCAS.
Did you question whether your symptoms were Histamine Intolerance or Mast Cell Activation Syndrome? We’d love it if you’d share with the community how you figured out which you were dealing with.
More About Histamine Intolerance and MCAS
- Mast Cells and Mast Cell Activation Syndrome 101
- What is Histamine Intolerance and How Can You Address It?
- Top Signs You Have Mold Toxicity
- The Best Antihistamine for Histamine Intolerance and Mast Cell Activation Syndrome
- MCAS Symptoms: Debunking Myths
Some links in this website are affiliate links, which means Mast Cell 360 may make a very small commission if you purchase through the link. It never costs you any more to purchase through the links, and we try to find the best deals we can. We only recommend products that we love and use personally or use in the Mast Cell 360 practice. Any commissions help support the newsletter, website, and ongoing research so Mast Cell 360 can continue to offer you free tips, recipes, and info. Thank you for your support!
References
Anyanwu, E. C., & Kanu, I. (2007). Biochemical impedance on intracellular functions of vitamin B12 in chronic toxigenic mold exposures. TheScientificWorldJournal, 7, 1649–1657. https://doi.org/10.1100/tsw.2007.113
Bankova, L. G. et al. (2016). The leukotriene E4 receptor, GPR99 mediates mast cell-dependent mucosal responses to the mold allergen, alternaria alternata. Journal of Allergy and Clinical Immunology. 137(2).
Chang, H. H., Chen, C. S., & Lin, J. Y. (2008). Dietary perilla oil inhibits proinflammatory cytokine production in the bronchoalveolar lavage fluid of ovalbumin-challenged mice. Lipids, 43(6), 499–506. https://doi.org/10.1007/s11745-008-3171-8
Doeun, D., Davaatseren, M., & Chung, M. S. (2017). Biogenic amines in foods. Food science and biotechnology, 26(6), 1463–1474. https://doi.org/10.1007/s10068-017-0239-3
Godman, H. (2021, August 1). Chronic gut inflammation: Coping with inflammatory bowel disease. Harvard Health. https://www.health.harvard.edu/diseases-and-conditions/chronic-gut-inflammation-coping-with-inflammatory-bowel-disease#:%7E:text=This%20gut%20inflammation%20may%20be,of%20new%20cases%20of%20IBD
Kempuraj, D., Castellani, M. L., Petrarca, C., Frydas, S., Conti, P., Theoharides, T. C., & Vecchiet, J. (2006). Inhibitory effect of quercetin on tryptase and interleukin-6 release, and histidine decarboxylase mRNA transcription by human mast cell-1 cell line. Clinical and experimental medicine, 6(4), 150–156. https://doi.org/10.1007/s10238-006-0114-7
Kritas, S. K., Gallenga, C. E., D Ovidio, C., Ronconi, G., Caraffa, A. l., Toniato, E., Lauritano, D., & Conti, P. (2018). Impact of mold on mast cell-cytokine immune response. Journal of biological regulators and homeostatic agents, 32(4), 763–768.
Li, Y., Yao, J., Han, C., Yang, J., Chaudhry, M. T., Wang, S., Liu, H., & Yin, Y. (2016). Quercetin, Inflammation and Immunity. Nutrients, 8(3), 167. https://doi.org/10.3390/nu8030167
Maintz, L., & Novak, N. (2007). Histamine and histamine intolerance. The American Journal of Clinical Nutrition, 85(5), 1185–1196. https://doi.org/10.1093/ajcn/85.5.1185
Mlcek, J., Jurikova, T., Skrovankova, S., & Sochor, J. (2016). Quercetin and its anti-allergic immune response. Molecules, 21(5), 623. https://doi.org/10.3390/molecules21050623
Nathan, N. (2018). Category: Mast Cell Activation. Retrieved from: https://neilnathanmd.com/category/mast-cell-activation/
Naviaux, R. K. (2014). Metabolic features of the cell danger response. Mitochondrion, 16, 7–17. https://doi.org/10.1016/j.mito.2013.08.006
Naviaux, R. K. (2020). Perspective: Cell danger response Biology—The new science that connects environmental health with mitochondria and the rising tide of chronic illness. Mitochondrion, 51, 40–45. https://doi.org/10.1016/j.mito.2019.12.005
Nuñez, M., del Olmo, A., & Calzada, J. (2016). Biogenic Amines. Encyclopedia of Food and Health, 416–423. https://doi.org/10.1016/b978-0-12-384947-2.00070-2
Pierron, A., Alassane-Kpembi, I., & Oswald, I. P. (2016). Impact of mycotoxin on immune response and consequences for pig health. Animal nutrition (Zhongguo xu mu shou yi xue hui), 2(2), 63–68. https://doi.org/10.1016/j.aninu.2016.03.001
Shin, T. Y., Kim, S. H., Kim, S. H., Kim, Y. K., Park, H. J., Chae, B. S., Jung, H. J., & Kim, H. M. (2000). Inhibitory effect of mast cell-mediated immediate-type allergic reactions in rats by Perilla frutescens. Immunopharmacology and immunotoxicology, 22(3), 489–500. https://doi.org/10.3109/08923970009026007
Yano, S., Umeda, D., Maeda, N., Fujimura, Y., Yamada, K., & Tachibana, H. (2006). Dietary apigenin suppresses IgE and inflammatory cytokines production in C57BL/6N mice. Journal of agricultural and food chemistry, 54(14), 5203–5207. https://doi.org/10.1021/jf0607361
Yano S., Umeda D., Yamashita T., Ninomiya T., Sumida M., Fujimura Y., Yamada K. and Tachibana H. (2007) Dietary flavones suppresses IgE and Th2 cytokines in OVA-immunized BALB/c mice. European Journal of Nutrition. 46 (257-263). https://doi.org/10.1007/s00394-007-0658-7




Patiently waiting to be a patient. – Peg Winsor
Thank you souch for this article! I was diagnosed almost 20 years ago by an astute diagnostician Immunologist who literally saved my life. At that time, Mastocytosis was the only category so the he made a ‘clinical’ diagnosis since my labs were normal but my symptoms fit everything else, choosing the right treatment and rescue remedy. I’ll be forever grateful to him. Now, 20 years later there have been enough people with symptoms for study that fall outside the parameters of Mastocytosis but are still very ill. I’ve had to do my own continuing education to be as healthy as I am today. I’m so grateful to have found your website to further my knowledge.
Hi Alice,
Thank you so much for reaching out! I’m so glad to hear the site has been helpful. Wishing you all the best!
While pregnant, I was diagnosed with Type B Strep. Upon birth, that Type B Strep immediately turned into mastitis. Words can’t express how horrid things were for me, as a new mother, trying to both breastfeed and nurture my baby. I have spent years wondering, and sometimes still wonder, if I am waiting for something else, medically associated to that mastitis to occur. Please include mastitis in your incredible documentation. Many women need knowledge and understanding of mastitis because of Type B Strep during pregnancy.
Hi Kristy, We are so sorry to hear you had to go through that and appreciate your suggestions for future content.
Hey,
Thanks for the write up. As someone who is suffering from several Lyme co-infections (but strangely enough, not Lyme), some mold exposure as well as SIBO, I am wondering how much of a role Mast Cell issues and/or histamine issues play. However, DAO medication and low histamine probiotics do not help, but seem to make me feel even worse, which is mystifying to me.
Do you ever hear of any patients where anti histamines/DAO medications and such exacerbate their symptoms?
Hi Nicklas,
Sorry to hear you are dealing with all of that. The short answer is, yes. In our sensitive community, nearly anything can be a trigger for somebody, it’s always possible. And there’s some trial and error to figuring out what is best for each person. With medications, it is very common for people to react to binders and fillers. You can read more about that here: https://mastcell360.com/best-antihistamine-for-histamine-intolerance/
Probiotics, even the low-histamine or lowering ones, can be touchy with all the gut issues that commonly accompany MCAS or histamine issues. You can read more about probiotics here: https://mastcell360.com/histamine-lowering-probiotics-for-people-with-mast-cell-activation-syndrome-and-histamine-intolerance/
And the conditions you listed are often contributors to MCAS and/or histamine issues. Mold is the #1 root cause contributor we see, and usually not the only thing adding to the issues. You can read more about all of that here: https://mastcell360.com/lyme-sibo-candida-ebv-in-mold-toxicity-why-wont-they-go-away-what-do-you-do-to-get-rid-of-them/
The search bar at the upper right of the website is a great way to find specific topics you’re interested in reading more about. Lots of terrific information available!
Best,
Kam
That is a good question. I had a terrible reaction to a DAO supplement. My test for the MCAS sympthoms on this site are over 100 points, so I do not undertand this either. And I already have fixed the mold and infection issues.