What Are Mast Cells? Mast Cell Activation Syndrome 101
In this blog post, we’re getting back to the basics on mast cells and Mast Cell Activation Syndrome (MCAS).
Are you just now learning about MCAS?
Or are you still figuring out how to deal with your MCAS?
Even if you’ve been following Mast Cell 360® for a while now, this should be a good refresher. I pick up new insights each time I hear something a second time. I hope you will, too!
Here’s what you’ll learn:
- What are mast cells?
- How does mast cell activation happen?
- What is Mast Cell Activation Syndrome?
- Symptoms of Mast Cell Activation Syndrome
- Top mast cell triggers that could be causing your reactions
- The connection between Mast Cell Activation Syndrome and mold
- The connection between Mast Cell Activation Syndrome and the nervous system
- The connection between Mast Cell Activation Syndrome and food intolerances
- What you can do for Mast Cell Activation Syndrome even if you are very sensitive
Okay, let’s get back to the basics… What are mast cells?
What Are Mast Cells?
It’s important you know that this blog post is for informational and educational purposes. It’s not meant to treat any health condition or to be prescriptive for anyone. If you have any medical condition, it is critical you work under the care and guidance of a licensed medical provider.
Different cell types perform different roles in your body.
Mast cells are white blood cells. They are specialized immune cells. And they perform many different roles.
What Is the Role of Mast Cells?
Mast cells have many roles and functions.
Here are just some of the roles mast cells are involved in:
- Immune function
- Defending against infections
- Detoxifying venom (bee sting, snake bite)
- Healing wounds and repairing tissue
- Helping to build connective tissues
- Balancing tissues and organs
- Supporting brain function
- Creating new brain cells
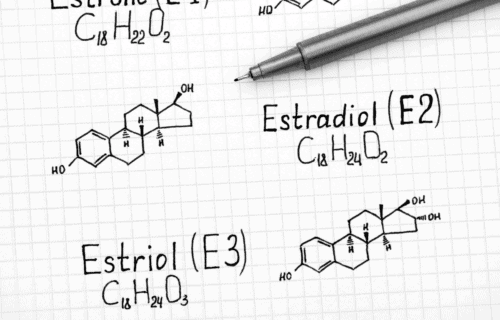
- Regulating the menstrual cycle
- Supporting fetal growth and placenta in pregnancy
One of the key mast cell roles you see listed is immune function.
I like to say that mast cells are some of the major conductors of the immune system. They are your frontline sensors and defenders.
Mast cells respond to everything both inside and outside your body.
They respond to:
- Pathogens (organisms that cause disease, like bacteria and viruses)
- Antigens (substances that trigger your immune response to make antibodies)
- Mold
- Candida
- Medications
- Hormones
- The nervous system
- Neurotransmitters
- Serotonin
- Dopamine
- Epinephrine
- Histamine
- Environmental factors
- Chemical exposure
- Temperature
- Light
- Odors
- Touch
- EMFs (electromagnetic fields)
Mast cells are found in almost every part of your body.
That’s why symptoms of MCAS can vary so widely. Keep reading to learn more about this.
Where Are Mast Cells in My Body?
Mast cells are found nearly everywhere except the retina. They usually aren’t found in the spinal cord, either. However, they can be found in the membrane surrounding the spinal cord.
The main categories of mast cell locations are:
- Mucosal and lining tissues
- Lining of the nose and sinuses
- Lining of the eyes
- Lining of the mouth
- Lining of the entire gastrointestinal tract (digestive tract)
- Lining of the bladder and urethra
- Lining of the lungs
- Blood vessel and cardiovascular tissues
- Arteries
- Veins
- Capillaries
- Heart
- Connective tissues
- Ligaments
- Tendons
- Bones
- Bone marrow
- Joints
- Lymphatic system
- Hair follicles
- Skin
- Nerve tissue and parts of the brain
Your mast cell related symptoms depend on which mast cells are triggered.
And that’s why your symptoms can seem so strange!
When I was really sick, even my hair follicles hurt.
It was a light bulb moment for me when I realized that Mast Cell Activation Syndrome was behind this!
You’ll read more about symptoms of MCAS coming up. But first, here’s what to know about how mast cells respond to triggers.
What Are Mast Cell Mediators and Receptors?
Below is a diagram of a mast cell. It’s from a study published in 2017.
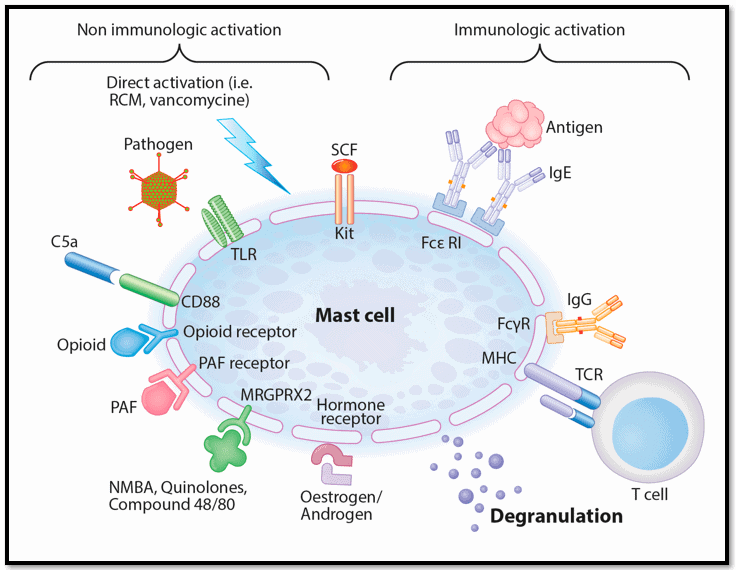
Image source: Spoerl, D., Nigolian, H., Czarnetzki, C., & Harr, T. (2017). Reclassifying anaphylaxis to neuromuscular blocking agents based on the presumed patho-mechanism: IgE-mediated, pharmacological adverse reaction or “innate hypersensitivity”?. International Journal of Molecular Sciences, 18(6), 1223. https://doi.org/10.3390/ijms18061223
This picture shows that your mast cells have several different kinds of receptors. This image is a simplified model. Mast cells actually have hundreds of receptors.
Mast cell receptors sense what’s happening in and around you. And from there, they communicate how the mast cells should respond.
(They can also communicate with other immune cells like T cells.)
These receptors play roles in:
- Allergic reactions
- Immune responses
- Food sensitivities
- Cell communications
- Stress responses
- And more
The mast cell response leads to a secretion of chemicals called mediators.
These mediators are communicators, too.
For example, histamine is one mediator. It signals inflammation. This is what leads to swelling, redness, and itching ─ common histamine related reactions.
You might experience these reactions when you come in contact with an allergen, for example. You may have even referred to these reactions as allergic reactions or allergic responses.
And if it is a true allergy, you are correct. But histamine release isn’t limited to allergic reactions alone. Your mast cells signal histamine release or any other mediator release as a response to any number of triggers.
FYI: Histamine Intolerance can be seen alongside Mast Cell Activation Syndrome because when mast cells are triggered, they can release histamine. Constant mast cell activation can lead to a steady stream of histamine in the body. If the body can’t keep up with eliminating this histamine, you can end up with Histamine Intolerance.
Mast Cell Degranulation
When the mast cells release these chemical mediators, that’s called mast cell degranulation.
The mast cells can release just a few of these chemicals. This is called partial or piecemeal degranulation.
Mast cells can also release all their mediators at once. This is called total degranulation.
There are over 200 different known mediators. But according to Mast Cell Activation Syndrome expert, Lawrence Afrin, MD, there may be over 1000 mediators!
There are different classes of mast cells mediators.
Common Mast Cell Mediators
Remember, there are a minimum of 200 known mast cell mediators. This list just gives you an idea. You may have heard some of these terms before.
Here are just a few mast cell mediators found in human mast cells:
- Biogenic amines
- Histamine (you’ve probably heard of this one the most!)
- Polyamines
- Serotonin
- Dopamine
- Lysosomal enzymes
- β-glucuronidase
- β-hexosaminidase
- N-acetyl β-glucosaminidase
- Cytokines and growth factors
- TNF (tumor necrosis factor)
- IL-4 (interleukin-4)
- SCF (stem cell factor)
- VEGF (vascular endothelial growth factor)
- Mast cell proteases
- Chymases
- Tryptases
- Tryptase-α
- Tryptase-βI
- Proteoglycans
- Heparin
- Chondroitin sulfates
- Serglycin
- Chemokines
- Leukotriene
- Prostaglandin
But here’s what you need to know: Mast cells are not the problem.
Your mast cells play an important role in your health.
In fact, there’s a rare disorder where people are born without mast cells. These people can’t survive in the world. If they do manage to survive, they have to live in a literal bubble.
So, you really do need your mast cells. You just want them to work FOR you – not against you. It’s only when mast cells become haywire that problems arise. Like Mast Cell Activation Syndrome.
You’ll learn more about that coming up.
But next, look at what Mast Cell Activation Syndrome really is and some of the more common symptoms of MCAS.
What Is Mast Cell Activation Syndrome?
With Mast Cell Activation Syndrome, you have a normal amount of mast cells. However, they are over-responsive.
Mast Cell Activation Syndrome is a dysregulation of the mast cells.
And this dysregulation is what causes problems.
When mast cells become overly responsive, they may react to real threats like bacteria and viruses. But they don’t quit responding when the threat has cleared.
Or they may start reacting to even safe things like certain foods or even medications.
There are two types of Mast Cell Activation Syndrome.
Clonal Mast Cell Activation Syndrome
Mast Cell Activation Syndrome can be genetic, or it can be acquired.
The rare, genetic form of Mast Cell Activation Syndrome is called clonal Mast Cell Activation Syndrome.
Non-Clonal Mast Cell Activation Syndrome
But the majority of Mast Cell Activation Syndrome is non-clonal. This means it’s not related to the mast cell genes.
Non-clonal MCAS isn’t rare. It’s thought that non-clonal MCAS may affect up to 17% of the general population.
And it affects about 50% of those with chronic health issues, if not more.
After the pandemic, we’re seeing this number rise due to Long Haul Syndrome.
Mast Cell Activation Syndrome is common in families because of:
- Genetic factors
- Environmental exposures (like toxic chemicals and mold)
Mast Cell Activation Syndrome vs Mastocytosis
Mast Cell Activation Syndrome is sometimes confused with Mastocytosis.
Mastocytosis is rare. It’s a mast cell disease in which there is an increased number of mast cells. It’s genetic.
You may also hear this called Systemic Mastocytosis.
Mast Cell Activation Syndrome is not Mastocytosis.
So, how do you know if you have Mast Cell Activation Syndrome?
Next read more about the diagnostic criteria for Mast Cell Activation Syndrome as well as the most common symptoms of MCAS.
Mast Cell Activation Syndrome Symptoms
When it comes to diagnostic criteria for Mast Cell Activation Syndrome, here’s what you need to know.
In Mast Cell Activation Syndrome, you’ll see an inflammatory response in at least 2 systems of the body. This is the minimum.
For example, you might have intestinal distress in your digestive system and joint pain in your musculoskeletal system.
Or you might have symptoms in your nervous system and respiratory system.
These are just two examples of how symptoms will show up in 2 different organ systems.
The list below shows some of the more common possible symptoms of Mast Cell Activation Syndrome. It doesn’t list everything. But it does show how Mast Cell Activation Syndrome can present in a lot of different ways!
Common Symptoms of Mast Cell Activation Syndrome
Which of these symptoms do you struggle with?
Systemic Symptoms
- Overall fatigue
- Inflammation
- Weight changes
- Sensitivities to
- Foods
- Medications
- Environment
- Toxic chemicals
- EMFs
- And more
Musculoskeletal Symptoms
- Osteoporosis
- Arthritis that moves around
- Muscle and/or bone pain
- Hyperflexible joints (it may or may not be Ehlers-Danlos Syndrome)
Skin Symptoms
- Itching
- Flushing
- Hives (Urticaria)
- Swelling (Angioedema)
- Rashes
- Hair loss
- Rosacea
- Psoriasis
- Eczema
Cardiovascular Symptoms
- Fainting or feeling faint
- Chest pains
- Heart palpitations
- Dizziness
- Low blood pressure
- Tachycardia (rapid heartbeat)
Digestive Symptoms
- Mouth burning
- Diarrhea
- Constipation
- Nausea
- Reflux
- Heartburn
- Food sensitivities
- IBS (Irritable Bowel Syndrome)
- Throat swelling
- Tongue swelling
- Abdominal pain or cramping
- Symptoms within 0 to 15 minutes of eating
Neurological Symptoms (Brain and Nervous System)
- Brain fog
- Difficulty paying attention
- Headaches
- Migraines
- Depression
- Anxiety
- Tingling
- Numbness
- Tinnitus
Lung and Respiratory Symptoms
- Congestion
- Coughing
- Shortness of breath
- Asthma
Reproductive System Symptoms
- Endometriosis
- Painful periods
- Male and female infertility
- Hormone imbalances
- Urinary symptoms like
- Inflammation
- Pain with urination
- Urinary tract infection type symptoms
You may also experience anaphylactoid or anaphylactic reactions. These can be life threatening.
Anaphylactic reactions might include:
- Difficulty breathing
- Constricted airway
- Hives
- Flushing or pale skin
- Weak and rapid pulse
- Nausea
- Vomiting
- Diarrhea
- Dizziness
- Fainting
- Rapid drop in blood pressure
- Sudden mental confusion
>>> Take the free Mast Cell Activation Symptoms Survey Here
Getting a diagnosis of MCAS can be hard, though. That’s because testing only catches about 10% of cases.
Instead, we often rely on symptoms to tell us what’s happening.
If the following is true for you, you may want to consider exploring Mast Cell Activation Syndrome further with your healthcare provider.
- Have you ruled out other conditions?
- Do you have mast cell activation symptoms in 2 or more systems?
- Have you seen improvement with removing triggers and supporting mast cells?
Speaking of mast cell triggers, just what are these triggers that evoke a mast cell response?
Mast Cell Triggers
You read earlier that your mast cells respond to everything inside and outside your body.
Technically, anything can trigger a mast cell response.
For most people without Mast Cell Activation Syndrome, these responses go unnoticed.
But if you have Mast Cell Activation Syndrome, it’s likely you have developed some hypersensitivities.
Have you ever felt like you react to EVERYTHING?
While it’s likely you aren’t literally reacting to everything, it can sure feel like it. That’s exactly how I felt for a long time!
Here are some of the top mast cell triggers I’ve seen:
- Toxic mold – this is the #1 trigger I see at the Mast Cell 360® practice
- Certain foods
- Toxic chemicals (such as fragrances, herbicides, pesiticides, etc.)
- Infections (bacterial like Lyme, viral like EBV (Epstein Barr), etc.)
- Hormone imbalances
- Lack of sleep
- Surgery
- Injuries
- Concussions
- Heavy metal toxicity
- Stress and trauma
- Certain genetics
Those are only a few possible triggers that may be behind some of your symptoms of MCAS.
But let’s go a little deeper with triggers. Let’s get to the root causes of Mast Cell Activation Syndrome.
Mast Cell Root Causes
There are a number of root causes we look at in the Mast Cell 360® practice.
You can get more information about these and other mast cell triggers by filling out the form below. (Click here if you don’t see the pink form.)
But right now, you can learn more about the top 3 root causes we see at Mast Cell 360®:
- 1. Mold Toxicity
- 2. Nervous system dysregulation
- 3. Food triggers
1. Mast Cell Activation Syndrome and Mold
First, let’s look at Mold Toxicity. It acts as a major trigger for the mast cells by:
- Dysregulating and dampening the immune response to bacteria and viruses
- Disrupting hormones
- Causing the nervous system to go haywire
- Clogging up detox pathways
- Disrupting the gut
Do you think mold might be an issue for you?
You can learn more about it in these articles on mold:
- How To Detox Your Body from Mold with MCAS
- Top Tips on Environmental Mold
- Mold Allergy vs Mold Toxicity
- Do You Have Mycotoxin Symptoms?
Mold Toxicity is the #1 trigger we see at Mast Cell 360®. It’s become an epidemic of sorts.
At this point, over 95% of the people who come through the Mast Cell 360® clinic have Mold Toxicity.
Looking into Mold Toxicity is very important if you are dealing with Mast Cell Activation Syndrome.
Mold is one of the worst triggers of Mast Cell Activation Syndrome and nervous system dysregulation.
Next let’s look at nervous system dysregulation. It’s another common root cause of MCAS.
2. Mast Cell Activation Syndrome and Your Nervous System
Nervous system dysregulation is where the fight, flight, or freeze and rest, heal, and repair parts of the nervous system get out of balance.
You can get stuck in fight, flight, or freeze. And this makes it very hard to rest, heal, and repair your body.
This kind of nervous system imbalance can cause all kinds of sensitivities. You can develop sensitivities to stimuli like light, sound, scents, and touch.
It can even cause issues with EMF, chemical, supplement, and medication sensitivities.
On top of this, many people with nervous system dysregulation have trouble with anxiety, depression, sleep, and mood swings.
Nervous system dysregulation can also be worsened by:
- Structural issues (like neck vertebrae out of balance)
- Fluid buildup on the brain
- Concussions
- Chiari malformation (where the brain drops into the hole in the skull for the spine)
- Stress
- Early traumas
- Lyme and coinfections
Related Post: Non Toxic Tick Prevention for People with Sensitivities
Symptoms of nervous system dysregulation in MCAS include:
- Difficulty falling asleep or staying asleep
- Easily stressed
- Easily startled
- Feeling wired or tired
- Anxiety, depression, or mood swings
- Constipation or diarrhea
- Sensitive to lights, sounds, touch, smells
- Sensitive to chemicals
- Sensitive to EMFs
- Food reactions
- Supplement or medication reactions
There are mast cells at every nerve ending. And the mast cells and nervous system work very closely together.
So, you can actually help your Mast Cell Activation Syndrome by working on your nervous system!
This is also why I call mast cells that have become over-sensitive haywire mast cells. It’s like the signaling gets mixed up.
You may just have mildly haywire mast cells. Or you may have severely haywire mast cells. The approach to fixing them is a little different depending on which category you’re in.
>>> Take the How Haywire Are Your Mast Cells Quiz Here
You can also learn more about what role the nervous system plays in Mast Cell Activation Syndrome and what you can do about it by reading these articles:
You can learn more about supporting your nervous system with the Mast Cell Nervous System Reboot here:
And, once you get your mast cells and nervous system calmed down, you can then try mast cell supporting supplements.
In my Top 8 Mast Cell Supporting Supplements Master Class, I cover not only my top favorite supplements, but I also give you tips on how to onboard each one.
And finally…let’s go over food triggers.
3. Mast Cell Activation Syndrome and Food Intolerances
Inflammatory foods are a very common trigger in Mast Cell Activation Syndrome. They can set off inflammation in your digestive system.
The main food trigger we think of with Mast Cell Activation Syndrome is high histamine foods.
However, lectins can also trigger mast cells. Knowing about lectins can be very important if you have any kind of autoimmunity or cancer history.
Some people can also be triggered by other food issues like Salicylates and FODMAPs. Especially in mold toxicity. But not everyone has trouble with these.
Don’t limit your foods unnecessarily.
And never limit them too much. This can lead to many other problems.
If you are working on changing your foods, be sure to work with your healthcare practitioner and don’t ever get too limited.
If you aren’t sure where to start, in my practice most people try eating low histamine for about 6 weeks to see if it makes a difference.
Some people notice they feel almost completely better after doing this. If that’s the case, you may only have Histamine Intolerance.
However, you may only notice some improvement. You may still have unresolved symptoms. That may be an indicator you have more going on than just Histamine Intolerance.
And it could very well be mast cell related.
If that’s the case, one of the next steps to consider with your health is looking at these other common food intolerances that occur with Mast Cell Activation Syndrome.
Many food intolerances are a result of overactive mast cells.
You can read about these additional food intolerances and triggers in the following posts:
- Histamine Intolerance
- Oxalate Intolerance
- Lectin Intolerance
- Salicylate Intolerance
- FODMAP Intolerance
If you are dealing with Mast Cell Activation Syndrome, the good news is that you can really improve when you start addressing those root factors.
And that’s what we’ll look at next…
How the MC360™ Method Addresses Mast Cell Activation Syndrome
You don’t have to deal with this forever. You really can improve your health. To do that, you’ll want to identify and address your underlying causes.
I do want you to know there aren’t any quick and easy answers to overcoming Mast Cell Activation Syndrome.
Medications can reduce symptoms in the short term. And medications can be a very important part of recovery.
But I want you to know that antihistamines and mast cell stabilizers don’t get rid of the underlying triggers.
Related Article: The Best Antihistamine for Histamine Intolerance and Mast Cell Activation Syndrome
So, if you only use medications, Mast Cell Activation Syndrome tends to get worse over the long-term. This is why you want to address the root causes.
It takes work, time, and dedication to recover. But I’m living proof that you can recover from Mast Cell Activation Syndrome.
I had Mold Toxicity, Lyme, Bartonella, Heavy Metals, Nervous System Dysregulation, and several other root triggers.
I was bedridden, couldn’t work, and barely able to hobble across the room with a cane. I had debilitating pain, fatigue, GI issues, and sensitivities to EVERYTHING.
I’ve recovered significantly.
So have the hundreds of clients I’ve worked with at Mast Cell 360®.
And I believe you can too!
I used my own experience and education to develop the MC360™ Method with the most sensitive people in mind.
Stabilization is the first step, and my Top 8 Supplements Course can help! Click below to learn more.
More Mast Cell Activation Syndrome Resources
- Histamine Intolerance vs MCAS
- My Favorite Mast Cell Friendly Products
- Mast Cell Foundations: Mediators and Receptors
Some links in this website are affiliate links, which means Mast Cell 360 may make a very small commission if you purchase through the link. It never costs you any more to purchase through the links, and we try to find the best deals we can. We only recommend products that we love and use personally or use in the Mast Cell 360 practice. Any commissions help support the newsletter, website, and ongoing research so Mast Cell 360 can continue to offer you free tips, recipes, and info. Thank you for your support!
References
Afrin, L. B. & Molderings, G. J. (2014a). A concise, practical guide to diagnostic assessment for mast cell activation disease. World Journal of Hematology, 3(1), 1. https://doi.org/10.5315/wjh.v3.i1
Afrin, L.B. (2013). Presentation, diagnosis, and management of mast cell activation syndrome. In: Murray, D.B. ed., Mast cells: phenotypic features, biological functions and role in immunity. MS, USA: Nova Science (pp. 155-232).
Akin, C., Valent P., & Metcalfe, D. D. (2010). Mast cell activation syndrome: Proposed diagnostic criteria. J allergy clin immunol, 126(6), 1099–104.e4. https://doi.org/10.1016/j.jaci.2010.08.035
da Silva, E. Z. M., Jamur, M. C., & Oliver, C. (2014). Mast cell function. Journal of Histochemistry and Cytochemistry, 62(10), 698–738. https://doi.org/10.1369/0022155414545334
Dahlin, J. S., & Hallgren, J. (2015). Mast cell progenitors: Origin, development and migration to tissues. Mol Immunol, 63(1), 9–17. https://doi.org/10.1016/j.molimm.2014.01.018
Gilfillan, A. M., Austin, S. J., & Metcalfe, D. D. (2011). Mast cell biology: introduction and overview. Adv Exp Med Biol, 716, 2–12. https://doi.org/10.1007/978-1-4419-9533-9_1
Hartmann, K., et al. (2016). Cutaneous manifestations in patients with mastocytosis: Consensus report of the European Competence Network on Mastocytosis; the American Academy of Allergy, Asthma & Immunology; and the European Academy of Allergology and Clinical Immunology. The Journal of Allergy and Clinical Immunology, 137(1), 35–45. https://doi.org/10.1016/j.jaci.2015.08.034
Jones, M. K., Nair, A. S., & Gupta, M. (2019). Mast cells in neurodegenerative disease. Frontiers in Cellular Neuroscience, 13. https://doi.org/10.3389/fncel.2019.00171
Krystel-Whittemore, M., Dileepan, K. N., & Wood, J. G. (2016). Mast cell: A multi-functional master cell. Frontiers in Immunology, 6, 620. https://doi.org/10.3389/fimmu.2015.00620
Lewis, C.A. (2016) Enteroimmunology. Carrabelle, Florida: Psy Press. (pp. 116-147).
Metcalfe D. D. (2008). Mast cells and mastocytosis. Blood, 112(4), 946–956. https://doi.org/10.1182/blood-2007-11-078097
Moon, T. C., Befus, A. D., & Kulka, M. (2014). Mast cell mediators: Their differential release and the secretory pathways involved. Frontiers in Immunology, 5, 569. https://doi.org/10.3389/fimmu.2014.00569
NHS. (2023, January 5). Mastocytosis. Natl Health Service, UK. Retrieved August 4, 2023, from https://www.nhs.uk/conditions/mastocytosis/
Spoerl, D., Nigolian, H., Czarnetzki, C., & Harr, T. (2017). Reclassifying anaphylaxis to neuromuscular blocking agents based on the presumed patho-mechanism: IgE-mediated, pharmacological adverse reaction or “innate hypersensitivity”?. International Journal of Molecular Sciences, 18(6), 1223. https://doi.org/10.3390/ijms18061223
Stone, K. D., Prussin, C., & Metcalfe, D. D. (2010). IgE, mast cells, basophils, and eosinophils. The Journal of Allergy and Clinical Immunology, 125(2 Suppl 2), S73–S80. https://doi.org/10.1016/j.jaci.2009.11.017
Theoharides, T. C., & Cochrane, D. E. (2004). Critical role of mast cells in inflammatory diseases and the effect of acute stress. Journal of Neuroimmunology, 146(1-2), 1–12. https://doi.org/10.1016/j.jneuroim.2003.10.041
Theoharides, T. C., et al. (2012). Mast cell activation and autism. Biochimica et Biophysica Acta, 1822(1), 34–41. https://doi.org/10.1016/j.bbadis.2010.12.017
Tshori, S., & Nechushtan, H. (2012). Mast cell transcription factors–regulators of cell fate and phenotype. Biochimica et Biophysica Acta, 1822(1), 42–48. https://doi.org/10.1016/j.bbadis.2010.12.024
Wernersson, S., & Pejler, G. (2014). Mast cell secretory granules: Armed for battle. Nature Reviews Immunology, 14(7), 478–494. https://doi.org/10.1038/nri3690



I want to hear more and I want to find this out , my doctor says my allergies are inside , new doctor I’am going to he is Indian and hard to understand , he said i have a Gene that’s from my Mom or Dad, it was hard to understand him he gave me some nose spray and helps with congestion but it comes back and he told me he wants me back if I still have trouble , he is a specialists my regular doctor wanted me to see him. I get very cold more that normal and can’t go out in the winter at all, lots of congestion and runs down my throat , my lung doctor gives me meds I inhale and says my asthma is not coming from my sinus’s, I have many problems
Hi Janice, We’re so sorry to hear that you are suffering with these symptoms. With MCAS, the most important thing is discovering your triggers, and the best thing you can do is to begin to remove and reduce exposure to such triggers. The most common trigger we see in the clinic is mold toxicity. You might find this blog helpful to see if that is something to consider addressing: https://mastcell360.com/top-signs-you-have-mold-toxicity-what-to-know-for-people-with-mast-cell-activation-syndrome-and-histamine-intolerance/