Mast Cell Foundations: Mediators and Receptors – info for those with Mast Cell Activation Syndrome or Histamine Intolerance
Whether you’re just now learning what MCAS (Mast Cell Activation Syndrome) and Histamine Intolerance are, or you’re at an advanced level, mast cells are complex. You probably still have a lot of questions!
Do you see terms like mast cell mediator or mast cell receptors and wonder just how that relates to what you are going through?
Or have you known about Mast Cell Activation Syndrome for a while but find yourself at a loss for words when you try to talk with your doctor about it?
This is totally understandable. There is a lot to know with Mast Cell Activation Syndrome! That’s why I want to go back to these essential foundations.
When you understand what’s happening with your mast cells, it’s easier to understand how certain things can trigger you. You can also better understand how to make good choices on what can help you!
Having some basic knowledge can make it easier to communicate with your practitioner about Mast Cell Activation Syndrome, too.
Today’s blog post will focus on mast cell mediators and receptors.
We’ll look at:
- What is a mast cell receptor?
- How are mast cells triggered?
- What is a mast cell mediator?
- What roles do receptors and mediators play in your reactions?
- And how can you start to manage overactive receptors and mediators?
Let’s start by looking at mast cells and mast cell receptors.
Related Article: Histamine Intolerance vs. Mast Cell Activation Syndrome: Do you have one, the other, or both?
What Are Mast Cells?
As part of understanding mast cell receptors, let’s look at what mast cells are.
Mast cells are a part of the immune system. They play several roles in your body. One we talk about frequently is the role they play in your immune response.
I like to think of them as guards of the castle gate, where the castle is your body. They stand guard and are prepared to fight off intruders like bacteria and other pathogens.
Mast cells are found in almost every part of the body.
Mast cells can be found in your:
- Skin
- Blood vessels
- Lymph vessels
- Nerve ending and brain
- Lungs and trachea
- Sinuses
- GI tract (including your mouth, esophagus, stomach, and intestines)
- Bladder and urethra
- Tendons and ligaments
- Bones
- Muscles
- Ears
- Eyes
Mast cells are just about everywhere except in the retina!
Mast cells are very important in maintaining good health.
Sometimes mast cells become over reactive and overly sensitive, though. At this point, the mast cells are dysregulated. I like to refer to this as “haywire” mast cells. When the mast cells are haywire, problems can arise.
So how do mast cells become haywire?
First, we need to understand more about mast cell receptors.
Mast Cell Receptors
The picture below is a simplified model that shows several kinds of mast cell receptors.
Receptors are part of cell signaling. They allow for communication between the cell and molecules outside of the cell.
Over 200 mast cell receptors have been described! This is how they can be so responsive to what is happening in and around your body. This makes them very complex cells!
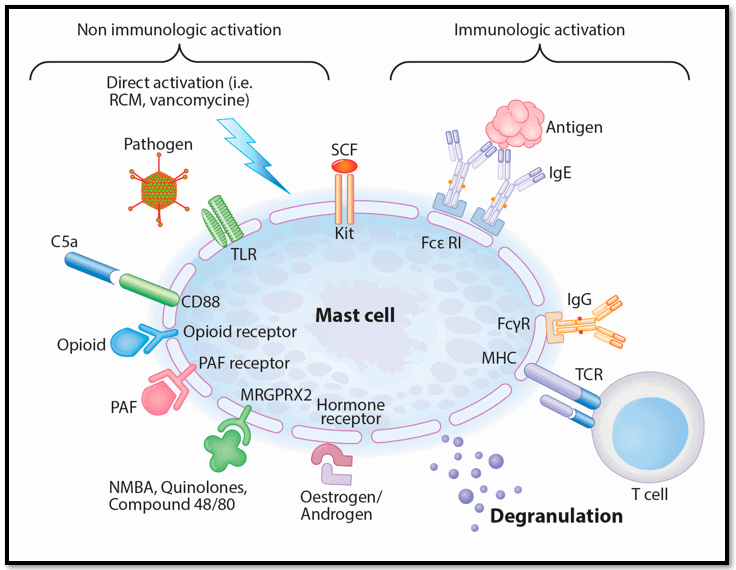
Image source: Spoerl, D., Nigolian, H., Czarnetzki, C., & Harr, T. (2017). Reclassifying Anaphylaxis to Neuromuscular Blocking Agents Based on the Presumed Patho-Mechanism: IgE-Mediated, Pharmacological Adverse Reaction or “Innate Hypersensitivity”?. International journal of molecular sciences, 18(6), 1223. https://doi.org/10.3390/ijms18061223
These mast cell receptors respond to everything you come in contact with. They are responding to everything outside and inside your body.
Your mast cell receptors can respond to:
- Temperature
- Vibrations
- Air you breathe
- Foods you eat
- Supplements
- Medications
- Hormones
- Neurotransmitters
For people without Mast Cell Activation Syndrome, many of these responses go unnoticed.
Some people with Mast Cell Activation Syndrome, though, can be very sensitive to certain foods or air pollution.
Some have trouble with changes in temperature, like getting too hot or cold. Some people can have trouble with vibrations from riding in a car on a bumpy road.
Some mast cell responses may make you feel better. For example, a response to a supplement or medication may signal the cells to stop releasing inflammatory chemicals.
Another example is that some neurotransmitters can calm mast cells. But neurotransmitters and hormones produced from stress may trigger mast cells.
Receptors can also respond to:
- Injuries (like a concussion)
- Pathogens
- Antigens (like a mold allergy)
- Mold and mold toxins (mycotoxins)
- Chemical toxins
- Candida
- Bacteria
- Viruses
- Stress and trauma
- EMFs
When the receptors respond, they release chemicals called mediators. We’ll talk more about those mediators soon.
But first, here’s a quick look at just a few of the better known mast cell receptors and their roles. This is just a small sampling of the over 200 receptors!
- FcεRI (pronounced Fc epsilon RI) – involved in IgE allergic reactions
- H1, H2, H3, and H4 histamine receptors – respond to histamine levels in different tissues of the body
- TLR (toll like receptors) – immune response to pathogens and lectins
- FcγR (pronounced Fc gamma R) – involved in IgG reactions (like food sensitivities)
- KIT receptor – responds to stem cell factor that drives how mast cells divide and grow; also important in the number of mast cells in the body
- Cytokine and T cell receptors – respond to communications from other types of immune cells
- CB1 (cannabinoid receptors) – respond to THC, CBD, CBG, etc.
- Hormone receptors – respond to hormones like estrogen and testosterone
- CRF receptors (Corticotropin releasing factor) – respond to stress, trauma
You can see, from just this small sampling, all the different communications mast cell receptors have with the whole body.
So…when these receptors are responding, we very broadly call that a mast cell response. Technically, any time a receptor responds to something, that’s a mast cell response. Mast cell responses happen all the time.
These responses can be very good. They can clean up infections and repair wounds. They can help with hormone and neurotransmitter balances. These responses protect and support our bodies every minute of every day.
But when we talk in terms of Mast Cell Activation Syndrome, we’re talking about when the mast cells receptors have become overly sensitive.
At this point, the hypervigilant and overresponsive mast cells aren’t responding in a normal way anymore. The mast cells are over-releasing the chemicals inside them.
We talk about this as mast cell reactions. Another way to talk about these reactions is called mast cell degranulation. We’ll get to degranulation in a bit. But to understand that process better, we first need to look at mast cell mediators.
Let’s look at that next.
Mast Cell Mediators and Inflammation
Mediators are the chemicals stored inside mast cells. Mediators play a lot of roles in your body, including defense and healing.
Here are just a few mediators and the roles they play. This is just a small list, though. It’s estimated there are over a thousand different types of mast cell mediators!
Histamine is the best know mediator. It has numerous roles, including being involved in inflammation and acting as a neurotransmitter.
Here are some others you may have heard of and some of their roles.
- Cytokines – inflammation increase, inflammation reduction, cell signaling
- Prostaglandins – blood vessel constriction or dilation
- Leukotrienes – blood vessel constriction or dilation
- Growth factors – growth of cells, new blood cell formation, blood vessel dilation
- Neurotransmitters and neuropeptides – signaling with the nervous system
- Tryptase – allergic responses and immunity
- Platelet activating factor – inflammation, anaphylaxis, platelet functioning, immune defense
Now, you may be wondering…if inflammation is a big problem, why is it part of healing and defense? First, I should mention not all mediators are inflammatory. Some are anti-inflammatory.
But inflammation isn’t all bad. It has a very important role in healing. In fact, it’s the first stage of healing.
It can cause small blood vessels to widen which allows more blood to reach injured tissue. The increased blood flow can also allow more immune cells to reach the injured area to help with healing.
It can also irritate the nerves to cause pain signals. Pain lets you know something is wrong so you can tend to the affected area.
Related Article: Pain in Mast Cell Activation Syndrome and Histamine Intolerance
Inflammation can also cause mucous membranes to release more fluid. Think: runny nose. That extra fluid is flushing toxins out of your body.
In someone with normally functioning mast cells, even inflammatory mediators are doing an important job.
Another thing to note in those with normally functioning mast cells is this: when the receptors sense the job is done, they signal the mast cells to stop releasing mediators.
But if you have Mast Cell Activation and your mast cells are haywire, here’s where problems can happen.
With haywire mast cells, the receptors don’t work like they should. (More on that when we talk about degranulation.) That means inflammation continues to be produced in your body. Chronic inflammation can be a problem.
Many symptoms are a result of chronic inflammation.
Serious chronic mast cell inflammation can show up as:
- Skin conditions like psoriasis, acne, urticaria, itching, swelling
- Gut issues like SIBO or IBS
- Joint and muscle pain
- Hypermobility and Ehlers-Danlos Syndromes
- Endometriosis
- Asthma
- Autoimmunity
And that’s just to name a few.
The mediator and mast cell location determine the types of symptoms you’re going to have.
For example, if the mast cells in your skin are over-releasing mediators, you’ll have skin symptoms.
If they are in your GI tract, you might have GI distress like acid reflux, diarrhea, or constipation.
You can also have heart palpitations related to the vagal nerve signaling to the heart.
Other symptoms include:
- Higher blood pressure
- Dizziness
- Chest pains
- Irritated eyes
- Mouth burning
- Difficulty breathing
There are so many possible MCAS symptoms resulting from the release of these mediators.
Now that you know a little more about mediators, let’s get back to the process of degranulation.
Degranulation
Mast cells keep their mediators housed in little bundles called granules.
Degranulation is the term for when the mediators inside the mast cells are being released as a response to a message from the mast cell receptors.
Here’s an example. A mast cell encounters an allergen. The receptor identifies it as a threat. It responds with mast cell degranulation – releasing chemicals (mediators) to deal with the threat.
In a person with normally functioning mast cells, once that original threat has been dealt with, the mast cell receptors signal for the mast cells to stop degranulating.
For those without Mast Cell Activation Syndrome, this process deals with the “danger” and then the body marks this as problem solved and goes back to business as usual.
For those with Mast Cell Activation Syndrome, this isn’t always the case.
If you have Mast Cell Activation Syndrome, it’s likely the receptors on your mast cells don’t properly control degranulation. In these cases, the mast cells continue to degranulate and become hyper-reactive. Your mast cells have gone “haywire.”
They keep releasing chemicals into the body even when they shouldn’t be doing so. This might be because the degranulation process doesn’t stop even after the initial stimulus has been dealt with.
It might also be because the mast cells start responding to things that aren’t really a threat. For some people, this might be certain foods, supplements, or even scents.
This can cause a wide range of symptoms in the body, and they often affect several systems at the same time. Because mast cells are found in so many locations in the body, the symptoms you get really depend on which mast cells are dysregulated.
So, what impairs the mast cells’ ability to control degranulation? There is usually an underlying cause for this kind of dysregulation.
Let’s look at that next.
Root Causes of Mast Cell Activation Syndrome
We talked about some of the things that receptors respond to. There’s no easier way to say this: some of those triggers keep on triggering!
Some of these are persistent threats. Mold Toxicity will continue to trigger the mast cells until it is addressed. The same with tickborne diseases like Lyme or Bartonella.
This is also true with chronic SIBO (small intestinal bacterial overgrowth), SIFO (small intestinal fungal overgrowth), candida, or chronic viral infections. As these kinds of pathogens rage on, inflammatory mediators continue to be released to protect you.
This can happen with stress, surgery, and even EMFs.
Food allergies and sensitivities can keep trigging mast cells. Pesticides and other chemicals in air, water, and food can keep triggering mast cells.
And chronic stress is a big one. Mast cells are particularly sensitive to what we think of as “normal, everyday stress.”
We live in a very stressful world. Just because we see this stress as normal doesn’t make it healthy.
Related Article: Resonant Breathing – the Mind-Body Connection
We also live in a world loaded with toxins in the air we breathe, in the water we drink, and in the food we eat.
No wonder Mast Cell Activation Syndrome has now been shown to be present in up to 17% of the Western population!
People with Mast Cell Activation Syndrome are what I like to think of as the “canaries in the coal mine”. Back in mining days, canaries were sent down the coal mines to make sure the air was safe.
Canaries were so sensitive they would pass out quickly if there were dangerous levels of carbon monoxide in the mines. This was a warning to the miners not to go down there.
The toxic world we live in is harming all of us. It’s just that some of us end up getting sick later in life with things like cancer.
But those of us with Mast Cell Activation Syndrome are the ones sounding the alarm for everyone else that what we’re living in isn’t safe! Our mast cell guards of the castle gate are sounding the alarm.
Fortunately, once these triggers are addressed, the mast cells can start to calm down again. You can stop flaring. You can stop reacting to so many things.
It’s amazing what can happen when you give your mast cells (and entire body) a break by living a healthy lifestyle! It takes a bit of work, but it’s well worth it. And, in doing this work, we can ward off many fatal diseases.
Here are just a few of the most common root causes I see:
Mold Toxicity
Mold Toxicity is the number one root cause of Mast Cell Activation Syndrome I see. Even if you aren’t in mold anymore, it can still be causing you problems.
Foods
Foods can also be a trigger. High histamine foods aren’t the only culprits here. Mast cells can also respond to lectins and many other foods if there are allergies, sensitivities, and intolerances.
Stress and Trauma
Stress and trauma is another root cause. A traumatic experience puts the body in the fight, flight, or freeze state (sympathetic nervous system). That sympathetic state triggers mast cells to activate. But, the parasympathetic state is significantly calming to mast cells.
Infections
Chronic Infection like Lyme, SIBO, or other ongoing infections will keep the mast cells on high alert, too.
There are others, too. All these triggers can cause the mast cells to go “haywire.”
And when the mast cells are haywire, they continue releasing mediators. Many of those mediators are inflammatory. When there is too much inflammation in the body, that can lead to problems.
So, what can you do? Keep reading to learn about some action steps to consider.
Be sure to work with a professional when you are making changes to your diet. You want to maintain proper nutrition and get as much variety as possible.
Learn more about the 7 most common Mast Cell Activation Syndrome root causes in your free report.
How Do You Support Yourself If You Have Mast Cell Activation Syndrome and “Haywire” Mast Cells?
Let’s look at root causes first.
Root Causes
The most important step you can take when you have Mast Cell Activation Syndrome is to address your underlying root causes.
Think about this analogy. You walk home every day through a thorn patch. You get cuts and scratches all up and down your arms. You can put ointment and bandages on those wounds. That takes care of the problem for a little bit. Those wounds start to heal.
But then you walk through the thorny plants again. You get more cuts and scratches. And the cuts from last time haven’t finished healing yet.
Each time, it just gets worse and worse, until your arms are an infected mess and you’re miserable.
Ultimately, you need to stop walking through that patch of thorny plants if you don’t want more scratches.
So, if you have Mold Toxicity, you need to detox the mold from your body and clear the mold from your environment.
Mold Toxicity weakens your body and throws the immune system out of balance. Mold toxins can also block your detoxification pathways.
This can lead to a number of challenges in your body. Here are just a few:
- Difficulty getting rid of chronic infections like Lyme and SIBO
- Sensitivities to everything from chemicals to supplements to foods
- Trouble with Vitamin D production (important for immune health)
- Significant mast cell activation
Related Article: How To Detox Your Body from Mold with MCAS
By addressing mold, your body’s immune system can start to get back in balance. That includes calming of the mast cells. Once this happens, your body can start addressing some of those issues like infections and sensitivities, and your mast cells should become less over responsive.
If food intolerances are causing your mast cells to be set off, you need to look at how you can change your diet to better support yourself. This might be by trying a low histamine diet.
Food intolerances can cause a lot of different reactions. Gut issues are among the most common reactions I see with this. Many of these gut issues are related to inflammation.
This is one of those downward spirals. Inflammation can trigger the mast cells to overrespond. Then, too high levels of inflammatory mast cell mediators can cause a lot more inflammation in the tissues.
This can trigger surrounding mast cells to get involved. And at that point, they start over releasing inflammatory mediators. I call this a mast cell cascade.
Whatever you call it, out of control mast cells are bad news for your body.
Getting the gut calmed down can help reduce inflammation and as a result, can calm the mast cell response.
If you have chronic stress and a dysregulated nervous system (and who doesn’t?), you need to work on things that calm your nervous system.
If you have trauma or PTSD, you may need counseling to help get you out of the sympathetic state (fight, flight, freeze) and into the parasympathetic state (rest, heal, digest.)
If your body is in sympathetic mode, it’s in an emergency state.
If your body thinks it’s under attack, your mast cells will be continuously releasing histamine and other inflammatory mediators.
Getting to the parasympathetic state can signal to the body that it isn’t under attack. Then it can start addressing healing.
Addressing those root factors is huge.
Supporting the nervous system is a very important first step in this process.
Related Post: The Link Between Concussions and Mast Cell Activation Syndrome
Supporting the Nervous System
I recommend all my clients start with addressing the nervous system. This is because there are mast cells at every nerve ending and in the brain.
Mast cells have receptors for neurotransmitters from the nerves. And nerves have receptors for mast cell mediators. There’s constant communication between the mast cells and the nervous system!
This is great news for you. It means even if you’re sensitive to everything, you can start calming the mast cells down by calming the nervous system.
Nervous system work has been a game changer for me and many of my clients.
It’s most effective to support 2 areas of the nervous system: the limbic system and the vagus nerve. This can be huge in helping to calm the mast cells from their dysregulated state.
I put together a class: Nervous System Reboot which will help you build your own roadmap to work through your personal needs when it comes to nervous system support.
I go over a lot of different support ideas that can help you at any stage. There are also some exercises included that you can get started with right away.
The next step is to work on supplements that remind the mast cells how to calm themselves back down again.
These supplements help reduce the sensitivity of the mast cell receptors. They can help minimize the effects of inflammatory mast cell mediators, too.
Let’s look at two of my favorite mast cell supporting supplements.
Baicalin
Baicalin is an extract of Chinese skullcap. Being an extract, it’s safer and more effective than full spectrum Chinese skullcap root.
Research has shown Baicalin can:
-
-
- Help suppress histamine release
- Inhibit mast cell degranulation
- Reduce airway inflammation
- Reduce mast cell involved nervous system inflammation
- Reduce IgE food responses
- Reduce various mediators
- Regulate signaling involved with chronic fatigue and adrenal fatigue
I love baicalin, particularly for supporting people with nervous system inflammation. That includes when there is anxiety, depression, sleep issues, heart palpitations, brain fog, etc.
Many of my Mast Cell 360 clients find it helps them a lot.
Not everybody tolerates baicalin, though. If you have salicylate intolerance, this may not be the right product for you.
I’ve also had some clients with chronic Lyme and a severe pathogen load who had to go super slow. This is because Baicalin has some gentle anti-microbial properties.
If you aren’t sure, talk with your provider with any questions or concerns. If you decide to try it, I suggest starting low and slow. You might have heard me say start with just drops or sprinkles.
One way to start would be by putting a sprinkle of it in water, stir it, and take a little sip of it. From there you can work up slowly.
If it goes well for you, it’s often taken at 250 milligrams twice a day.
TIP: It can be taken with food or about 30 minutes before meals.
You can use coupon code MASTCELL10 for 10% off!

Perimine
Perimine is perilla seed extract. Perilla is an herb used in Asian cooking.
You might have eaten it before if you eat Thai, Korean, or Vietnamese food.
As a supplement, research has shown that perilla seed extract specifically has a lot of benefits for mast cells.
Here are a few of the ways the research showed it can help:
-
- Reduce histamine
- Reduce the TNF alpha cytokine
- Reduce inflammation
- Help skin allergic reactions
- Improve respiratory symptoms
It’s lower salicylate than the baicalin. Again, though, talk with your provider with any questions or concerns. And remember…start low and slow.
Eventually, as tolerated, you can consider working up to one tablet or one capsule up to three times per day. I take it 30 minutes before meals. It helps calm the GI tract before eating.
TIP: 4 tablets/day is the max. 1 tablet 30 minutes before meals is usual, but in a flare, a 4th tablet taken at some point in the day may be helpful.

Register with FullScript to get 15% off Perimine!
These are some ways you can start to deal with those mast cell reactions caused by oversensitive receptors and the mediators they release.
You can learn about more supplements that can support your mast cells here:
I hope this “back-to-basics” has been helpful!
More Mast Cell Resources
References
Britannica, T. Editors of Encyclopaedia (2018, December 6). mast cell. Encyclopedia Britannica. https://www.britannica.com/science/mast-cell
Bui, T. T., Piao, C. H., Song, C. H., Lee, C. H., Shin, H. S., & Chai, O. H. (2017). Baicalein, wogonin, and Scutellaria baicalensis ethanol extract alleviate ovalbumin-induced allergic airway inflammation and mast cell-mediated anaphylactic shock by regulation of Th1/Th2 imbalance and histamine release. Anatomy & cell biology, 50(2), 124–134. https://doi.org/10.5115/acb.2017.50.2.124
da Silva, E. Z., Jamur, M. C., & Oliver, C. (2014). Mast cell function: a new vision of an old cell. The journal of histochemistry and cytochemistry : official journal of the Histochemistry Society, 62(10), 698–738. https://doi.org/10.1369/0022155414545334
Hennino, A., Bérard, F., Guillot, I., Saad, N., Rozières, A., & Nicolas, J. F. (2006). Pathophysiology of urticaria. Clinical reviews in allergy & immunology, 30(1), 3–11. https://doi.org/10.1385/CRIAI:30:1:003
Isis M. (1998). The golden root: Clinical applications of Scutellaria baicalensis Georgi flavonoids as modulators of the inflammatory response. Alternative Medicine Review, 3, 472-480. 62.
Kim, D. S., Son, E. J., Kim, M., Heo, Y. M., Nam, J. B., Ro, J. Y., & Woo, S. S. (2010). Antiallergic herbal composition from Scutellaria baicalensis and Phyllostachys edulis. Planta medica, 76(7), 678–682. https://doi.org/10.1055/s-0029-1240649
Krystel-Whittemore, M. (2016). Mast Cell: A Multi-Functional Master Cell. Frontiers. Retrieved January 14, 2022, from https://www.frontiersin.org/articles/
10.3389/fimmu.2015.00620/full
Lenhard, E., & Moeser, A. (2018, December 19). Don’t Overreact: Research Pinpoints Mast Cell Receptor in Immune Response, Disease Signs. The College of Veterinary Medicine at Michigan State University. Retrieved January 14, 2022, from https://cvm.msu.edu/news/2018/dont-overreact-research-pinpoints-mast-cell-receptor-in-immune-response-disease-signs
Liu, Y. H., Lu, M., Xie, Z. Z., Hua, F., Xie, L., Gao, J. H., Koh, Y. H., & Bian, J. S. (2014). Hydrogen sulfide prevents heart failure development via inhibition of renin release from mast cells in isoproterenol-treated rats. Antioxidants & redox signaling, 20(5), 759–769. https://doi.org/10.1089/ars.2012.4888
Makino T, Furuta Y, Wakushima H, Fujii H, Saito K and Kano Y. (2004). Antiallergic effect of Perilla frutescens and its active constituents. Phytotherapy Research. 17, 240-243.
Makino T, Furuta Y, Wakushima H, Fujii H, Saito K and Kano Y. (2001). Effect of oral treatment of Perilla frutescens and its constituents on type-I allergy in mice. Biological and Pharmaceutical Bulletin, 24(10), 1206-1209.
Moon, T. C. (2014). Mast Cell Mediators: Their Differential Release and the Secretory Pathways Involved. Frontiers. Retrieved January 14, 2022, from https://www.frontiersin.org/articles/10.3389
/fimmu.2014.00569/full
Mukai, K., Tsai, M., Saito, H., & Galli, S. J. (2018). Mast cells as sources of cytokines, chemokines, and growth factors. Immunological reviews, 282(1), 121–150. https://doi.org/10.1111/imr.12634
Sanbongi C, Takano H, Osakabe N, Sasa N, Natsume M, Yanagisawa R, Inoue K-I, Sadakane K, Icinose T and Yoshikawa T. (2004). Rosmarinic acid in perilla extract inhibits allergic inflammation induced by mite allergen, in a mouse model. Clinical & Experimental Allergy, 34, 971-977.
Sandig, H., & Bulfone-Paus, S. (2012). TLR signaling in mast cells: common and unique features. Frontiers in immunology, 3, 185. https://doi.org/10.3389/fimmu.2012.00185
Savage, K., Firth, J., Stough, C., & Sarris, J. (2018). GABA-modulating phytomedicines for anxiety: A systematic review of preclinical and clinical evidence. Phytotherapy research : PTR, 32(1), 3–18. https://doi.org/10.1002/ptr.5940
Shin, T. Y., Kim, S. H., Kim, S. H., Kim, Y. K., Park, H. J., Chae, B. S., Jung, H. J., & Kim, H. M. (2000). Inhibitory effect of mast cell-mediated immediate-type allergic reactions in rats by Perilla frutescens. Immunopharmacology and immunotoxicology, 22(3), 489–500. https://doi.org/10.3109/08923970009026007
Spoerl, D., Nigolian, H., Czarnetzki, C., & Harr, T. (2017). Reclassifying Anaphylaxis to Neuromuscular Blocking Agents Based on the Presumed Patho-Mechanism: IgE-Mediated, Pharmacological Adverse Reaction or “Innate Hypersensitivity”?. International journal of molecular sciences, 18(6), 1223. https://doi.org/10.3390/ijms18061223
Sowndhararajan, K., Deepa, P., Kim, M., Park, S. J., & Kim, S. (2018). Neuroprotective and Cognitive Enhancement Potentials of Baicalin: A Review. Brain sciences, 8(6), 104. https://doi.org/10.3390/brainsci8060104
Takano, H., Osakabe, N., Sanbongi, C., Yanagisawa, R., Inoue, K., Yasuda, A., Natsume, M., Baba, S., Ichiishi, E., & Yoshikawa, T. (2004). Extract of Perilla frutescens enriched for rosmarinic acid, a polyphenolic phytochemical, inhibits seasonal allergic rhinoconjunctivitis in humans. Experimental biology and medicine (Maywood, N.J.), 229(3), 247–254. https://doi.org/10.1177/153537020422900305
Thangam, E. B. (2018). The Role of Histamine and Histamine Receptors in Mast Cell-Mediated Allergy and Inflammation: The Hunt for New Therapeutic Targets. Frontiers. Retrieved January 14, 2022, from https://www.frontiersin.org/articles/
10.3389/fimmu.2018.01873/full
Theoharides, T. C., Donelan, J. M., Papadopoulou, N., Cao, J., Kempuraj, D., & Conti, P. (2004). Mast cells as targets of corticotropin-releasing factor and related peptides. Trends in pharmacological sciences, 25(11), 563–568. https://doi.org/10.1016/j.tips.2004.09.007
Trinh, H. T., Joh, E. H., Kwak, H. Y., Baek, N. I., & Kim, D. H. (2010). Anti-pruritic effect of baicalin and its metabolites, baicalein and oroxylin A, in mice. Acta pharmacologica Sinica, 31(6), 718–724. https://doi.org/10.1038/aps.2010.42
Ueda, H., Yamazaki, C., & Yamazaki, M. (2002). Luteolin as an anti-inflammatory and anti-allergic constituent of Perilla frutescens. Biological & pharmaceutical bulletin, 25(9), 1197–1202. https://doi.org/10.1248/bpb.25.1197
Xu, H. (2020, November 25). Neurotransmitter and neuropeptide regulation of mast cell function: a systematic review – Journal of Neuroinflammation. BioMed Central. Retrieved January 14, 2022, from https://jneuroinflammation.biomedcentral.com/
articles/10.1186/s12974-020-02029-3
Xu, L., Li, J., Zhao, P., & Zhang, X. (2017, August 17). Regulatory effect of baicalin on the imbalance of Th17/Treg responses in mice with allergic asthma. ScienceDirect. Retrieved January 14, 2022, from https://www.sciencedirect.com/science/article/
abs/pii/S0378874117306840
Yun, M. (2020, June 29). Enriched-Baicalein Attenuates Allergy in Cells and Mice. Hindawi. Retrieved January 14, 2022, from https://www.hindawi.com/journals/ecam
/2020/4780210/
Zimmerman, G. A., McIntyre, T. M., Prescott, S. M., & Stafforini, D. M. (2002, May). The platelet-activating factor signaling system and its. . . : Critical Care Medicine. LWW. Retrieved January 14, 2022, from https://journals.lww.com/ccmjournal/Abstract
/2002/05001/The_platelet_activating_factor_
signaling_system.20.aspx
InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. What is an inflammation? 2010 Nov 23 [Updated 2018 Feb 22]. Available from: https://www.ncbi.nlm.nih.gov/books
/NBK279298/




Hi Beth,
I am curious, if I react to BAD to Tyramines, can I try either of these recommended supplements ? You mentioned how people who react to salicylates may have issues with them. How about Tyramines?
Thanks SOOO much for all you share with us. Love your insights and recommendations! ~
Leslie
Hi Leslie,
These supplements are low tyramines, which are a very different compound than salicylates. You’ll want to talk with your practitioner who knows your history with any questions or concerns. Thanks for your interest in Mast Cell 360!