
Mast Cell Activation Syndrome and Ehlers-Danlos Syndrome
My husband and I used to joke that my body was held together with duct tape and popsicle sticks.
This may sound familiar to you if you’ve been dealing with Mast Cell Activation Syndrome (MCAS) and Hypermobile Ehlers-Danlos Syndrome (hEDS), too.
I sported a lot of Kinesio tape and joint braces to help support my body.
The Kinesio tape offered me some pain relief and supported muscle movement.
With both MCAS and hEDS, I had a lot of joint pain and muscle pain.
And with hEDS, my skin was so stretchy that it would peel off when I removed the Kinesio tape.
Now, you might think that with hypermobility, I was extra flexible. Or you may think that you don’t have hEDS because you aren’t flexible.
But that isn’t necessarily true.
Yes, my knees and elbows hyperextended.
But when I started yoga, I couldn’t do the poses like they were demonstrated.
I couldn’t touch my toes or the floor. I could barely even touch my knees!
That’s because my muscles were so spasmed trying to hold my loose joints together.
In fact, years later, I realized that stretching was making me worse.
So, you may be surprised to hear that even though I was being held together with tape and braces, I reversed my hEDS.
My osteopath was shocked!
Keep reading for the rest of my story and to learn more on:
- What is Ehlers-Danlos Syndrome (EDS)?
- Signs you may have Ehlers-Danlos Syndrome
- Causes of EDS
- The links between MCAS, EDS, and mold
- Testing for EDS
- What you can do to reverse or improve EDS
What Is Ehlers-Danlos Syndrome?
It’s important you know that this blog post is for informational and educational purposes. It’s not meant to treat any health condition or to be prescriptive for anyone. If you have any medical condition, it is critical you work under the care and guidance of a licensed medical provider.
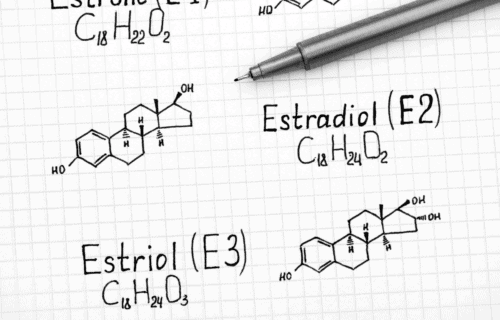
Ehlers-Danlos Syndrome is a set of connective tissue disorders.
Connective tissues support your organs and hold your body together. These tissues are made of collagen and elastin. These are proteins.
EDS affects your body’s ability to produce collagen. This means that with EDS, your connective tissue can be compromised.
Ehlers-Danlos Syndrome can affect the connective tissues that support:
- Skin
- Bones
- Blood vessels
- Organs
- Muscles
- Tendons
- Ligaments
- Other tissues
There are different types of EDS. It’s unlikely that you would have more than 1 type. However, it is possible to have symptoms that are seen across the different types.
The following are very rare subtypes of EDS.
After you take a look at some of the rare forms below, keep reading to learn more about the more common types, including Hypermobile EDS.
Hypermobile type EDS is what I’ve dealt with. And I’ll share more with you on the links between hEDS and Mast Cell Activation Syndrome, too.
But first, here’s a quick rundown on the rare genetic forms of Ehlers-Danlos Syndrome.
Rare Forms of Ehlers-Danlos Syndrome
Each of these rare types of EDS are genetic. And they each have different distinguishing features and associated genes.
Some symptoms associated with these types of EDS can be serious and life-threatening.
You might experience issues with your vision, hearing, heart, breathing, and even your head and facial bones.
It’s important to talk with your doctor if you have a history of these rare diseases in your family.
Some of the rarer types of EDS, that affect only about 1 in 1,000,000, people include:
- Arthrochalasia EDS
- Brittle Cornea Syndrome
- Cardiac-valvular EDS
- Classical-like EDS
- Dermatosparaxis EDS
- Kyphoscoliotic EDS
- Musculocontractural EDS
- Myopathic EDS
- Periodontal EDS
- Spondylodysplastic EDS
Those are the rarer forms of EDS.
Another type of EDS is Vascular EDS (vEDS).
This type of EDS can affect all cardiovascular vessels. And it can cause aortic dysfunction.
The aorta is your largest artery. It moves blood from your heart to the circulatory system.
Aortic dysfunction can be deadly. So, it’s very important to talk with your doctor if you have a history of this in your family.
This isn’t as rare as the other forms listed above. But it isn’t as common as the 2 you’ll read about next.
Common Types of EDS
There are also more common types of EDS including:
- Classical EDS
- Hypermobile EDS
Let’s take a closer look at these types next.
Classical EDS
Classical EDS is different from Classical-like EDS (the rarer type). Both are genetic types.
One thing that distinguishes them is the associated genes — TNXB (Classical-like EDS) and COL5A1, COL5A2, and COL1A1 (Classical EDS).
Classical EDS affects an average of 1 in 30,000 people.
Symptoms of EDS, Classical type, include:
- Very stretchy skin
- Fragile skin
- Scarring below the normal layer of skin tissue
- Joint hypermobility (overly flexible joints)
Can you relate to any of the other diagnostic criteria for Classical type EDS that include:
- Smooth, velvety skin
- Bluish-grey, spongy nodules associated with scars over pressure points and areas like the elbows and knees
- Small, hard nodules that are movable under the skin
- Complications of joint hypermobility (sprains, dislocations, subluxations)
- Weak or decreased muscle tone (Hypotonia)
- Easy bruising
- Tissue fragility
- Surgical complications (such as postoperative hernias)
- Positive family history
Hypermobile EDS (hEDS)
Many contortionists or gymnasts who don’t train for their flexibility often have undiagnosed Hypermobile EDS.
I had a client who was a circus performer with genetic EDS. She was in a wheelchair by age 35 due to the excessive exertion.
And her issues were compounded by severe osteoporosis related to Mold Toxicity and MCAS.
But hEDS doesn’t just affect athletes.
Hypermobile EDS is the type of EDS that I’ve dealt with. It’s the most common type. Studies show that it affects an average of about 1 in 4,000 people.
However, specialists in this area suspect it is much more common and underrecognized.
You have an increased risk of injury due to joints being too flexible if you have hEDS.
You may also be at increased risk for:
- Abdominal cramping, bloating, loose stools, or constipation
- Anxiety
- Bladder problems
- Chronic pain
- Dizziness when standing up
- Easy bruising
- Feeling tired
- Joint problems such as arthritis and dislocation
- Problems with skin healing (scars) or wound healing
Telltale signs of hEDS include:
- Generalized joint hypermobility
- Joint instability
- Chronic pain
- Stretchy skin (less stretchy than other forms of EDS, but skin can still tear easily)
These types of symptoms can definitely impact your quality of life.
There was a time when my dog pulled on the leash while I was walking her. My shoulder dislocated.
I couldn’t get deep tissue massage to aid in pain relief. (It made me feel worse!)
Stubbing my toe caused dislocation.
I couldn’t carry anything over 10 pounds. This made travel and grocery shopping extremely difficult.
And the pain added to my insomnia.
These are just a few of the ways I was impacted.
How has EDS impacted the quality of your life?
Is hEDS Genetic, Too?
All of the other types of EDS you’ve read about are genetic.
Some researchers and practitioners are considering that there may be a genetic component to the hypermobility type.
It is thought that, if it is genetic, hEDS may be autosomal dominant. That means you can get the disease if even just one parent carries the gene abnormalities.
But currently, there is no gene to test for hEDS. So, we aren’t sure if it may be a mix of genetic and secondary or all secondary.
It’s been observed that there is a tendency for hEDS to run in families. This could mean there is a genetic component.
But it could be due to a shared environment where all family members are exposed to the same environmental triggers.
For example, shared exposure to mold and mycotoxins or pets with fleas carrying Bartonella.
So, we often refer to this form of EDS as “acquired”. Meaning it isn’t genetic. Rather, it is acquired due to secondary factors like:
- MCAS
- Mold Toxicity
- Bartonella
Here’s what’s interesting about hEDS, though.
It’s possible to reverse hEDS if you address those secondary factors, or root triggers.
When I addressed those root triggers, my osteopath found no signs of hEDS anymore!
Let’s look more at these common root triggers of hEDS next.
Root Triggers of Hypermobile Ehlers-Danlos Syndrome (hEDS)
There was a lot I didn’t know when I was trying to get my health back. Little by little, I started putting the pieces together.
I cleaned up my diet and addressed my food intolerances.
I started getting my mast cells calmed down with nervous system supports and mast cell supporting supplements.
I was able to uncover some chronic infections I’d been dealing with and address those.
And I started addressing Mold Toxicity.
What I didn’t know is that doing all these things was going to help my hEDS, too.
I’ve since learned why addressing these root triggers of MCAS also turned out to be addressing my root triggers of hEDS.
Here’s more on that.
Bartonella
Bartonella is a bacteria spread to humans by fleas, body lice, sand flies, or contact with flea-infested animals.
We also commonly refer to infection from these bacteria as Bartonella.
Bartonella bacteria can upset your red blood cells, immune cells, and the cells lining your blood vessels.
In this way, Bartonella can contribute to Mast Cell Activation Syndrome.
It can also contribute to connective tissue degradation, like what is experienced with Ehlers-Danlos Syndrome.
Mast Cell Activation Syndrome
Any type of infection or disease can trigger mast cell activation.
Normally functioning mast cells will stop responding once the threat has been dealt with.
But if have haywire mast cells, they can remain overly reactive even once the threat is gone.
But what if you have chronic infections like Bartonella or Lyme?
Your mast cells stay active trying to fight these threats and protect you.
Infections aren’t the only thing that can trigger mast cells though.
Related Post: What Is MCAS?
Whatever the cause of your MCAS, here’s what happens when your mast cells are responding.
Your mast cell receptors sense what’s going on. For example, bacteria enter your system.
It identifies this as a threat and responds accordingly. They respond by releasing mediators. This is part of a process called mast cell degranulation.
Mediators are chemicals stored inside mast cells. They play a lot of different roles in your body, particularly in regard to defense and healing.
There are over 1,000 known mast cell mediators.
Histamine is one of the most well-known.
Another one of these mediators is Elastase-2. This inflammatory mediator affects connective tissue.
So, more mast cell activation means more mediators will be released.
And over time, it’s this surplus of Elastase-2 mediator that can break down proteins that affect connective tissues.
In other words, too many inflammatory mediators can hurt your joints.
Additionally, Bartonella and mycotoxins break down connective tissues directly. And both of these are common root causes of MCAS.
Mold Toxicity
Mold Toxicity is the #1 root cause of Mast Cell Activation Syndrome we see in the Mast Cell 360 practice.
Mold releases toxins called mycotoxins.
These mycotoxins wreak all kinds of havoc on your nervous system, your immune system, your digestive system, and so much more.
Another thing mycotoxins do? They degrade connective tissue by digesting tissues to get the nutrients. That leaves you depleted in nutrients needed to build connective tissue.
According to Neil Nathan, MD, mold toxins can essentially move through any body tissue at will. This means your connective tissues are extremely prone to be harmed by these toxins.
You can learn more about how to address mold in my MC360® Precision Mold Master Class.
Other Connections Between MCAS, EDS, and More
Andrew Maxwell, MD, a pediatric cardiologist, kept noticing that patients who had mast cell activation often had 5 affiliated conditions.
He called these the PENTAD conditions (pent meaning 5). These are:
- Hypermobile Ehlers-Danlos Syndrome (hEDS)
- Mast Cell Activation Disorder (MCAD) / Mast Cell Activation Syndrome (MCAS)
- POTS (Postural Orthostatic Tachycardia Syndrome) / Dysautonomia
- Autoimmunity
- Gastroparesis (slow movement of food from your stomach to your small intestine)
In a recent interview I did with Kelly McCann, MD, she said that it’s really helpful for practitioners to understand the overlapping nature of these conditions.
For example, if you live in a moldy environment, it’s more likely to trigger your MCAS. Additionally, if you have MCAS and hypermobile connective tissue, mycotoxins and mast cell activation can further increase hypermobility.
This can lead to amped up hEDS and even other conditions like CCI (Craniocervical Instability) or MALS (Median Arcuate Ligament Syndrome).
So, now that you know a little more about the types of Ehlers-Danlos Syndrome, the next question may likely be how can I test for it?
Keep reading to learn more. Then I’ll share more details with you on how I reversed hEDS and what you can consider, too.
But first, here’s more on testing for Ehlers-Danlos Syndrome.
Testing for Ehlers-Danlos Syndrome
For the genetic types of EDS, you can get a diagnosis via genetic testing by a medical geneticist.
This is a very specialized blood test. You won’t be able to determine this with a saliva test like 23andMe.
There is no genetic testing for Hypermobility type EDS, at this time.
Clinical assessment to determine hEDS can include the Beighton test.
The Beighton Test
The Beighton Scoring System measures joint hypermobility on a 9-point scale.
The joints assessed in the Beighton Test are:
- Knuckle of both pinky fingers – Can the pinky finger bend backwards 90 degrees or more?
- Base of both thumbs – Can the thumbs bend down to touch the underside of your forearm?
- Elbows – With arms outstretched and palms facing upwards, does the elbow extend upwards more than an extra 10 degrees?
- Knees – While standing, with knees locked, does the lower part of the leg extend more than 10 degrees forward?
- Spine – Can the palms of your hands touch the floor without bending your knees?
How many did you answer yes to?
Answering yes to 2 or more of the questions above may be an indicator you have hEDS.
The Beighton Test alone has limitations, though.
Hypermobile type EDS can be expressed in more joints than those assessed by Beighton.
It can affect:
- Hips
- Ribs
- Wrists
- Ankles
- And more
And it is possible to be hypermobile and not have hEDS. Some people have a less serious condition called HSD (Hypermobility Spectrum Disorder).
Alena Guggenheim, ND, stated that when screening for hEDS, she considers the following, too:
- Chronic joint instability – even starting back in childhood, which can be recurrent ankle sprains, kneecap dislocations, shoulder dislocations, etc
- Chronic pain – not necessarily just in areas of joint instability
- Fatigue – very common in this population
- Gastrointestinal symptoms – intestines are made of and held in place by connective tissues
- Allergic disorders – growing evidence suggests that some EDS patients have comorbid immunodeficiencies and/or allergic disorders
- Postural symptoms – achiness, feeling of “heavy body” or like it’s work just to sit up with good posture
- Autoimmunity – when your body attacks its own healthy cells and tissues
What To Do About hEDS
I mentioned earlier that my osteopath was shocked when I showed no more signs of EDS. He wanted to know what I had been doing for my health.
I had been working on the common triggers:
- Addressing Mast Cell Activation Syndrome and getting my mast cells calmed down
- Detoxing from mycotoxins (mold toxins)
- Addressing Bartonella (a bacterial infection)
These were some of the root causes of my chronic pain and tissue damage.
Getting these things handled went a long way to reversing EDS.
Here are some of my other top tips for reversing hEDS.
Address Food Triggers
Before you change your diet on your own, please make sure you’re working with a healthcare practitioner who can help you with this. Never limit foods unnecessarily, and always have a licensed medical provider who is supervising your case.
Lots of foods can trigger mast cells if you have Mast Cell Activation Syndrome.
These intolerances or sensitivities can include:
- High Histamine Foods
- Lectins
- Oxalates
- Salicylates
- And more
Evaluating your diet to address food triggers can help calm the mast cells.
But it’s very important to remember that not everyone has all of these food triggers. So don’t reduce your foods unnecessarily.
When it comes to food, it’s also important to support good nutrient balance. You need a variety of nutrients to support good health.
Work with a nutritionist or health care professional to be sure you are getting a well-balanced, nourishing diet that addresses your unique needs and triggers.
Learn more about the Low Histamine Diet in this post.
Support Connective Tissue
Supplements alone won’t reverse EDS. You absolutely must address your triggers, too.
But supplements can help by:
- Supporting mast cells
- Aiding with tissue repair and building
Here are some of the top supplements I recommend for supporting your body as you tackle EDS.
Vitamin C
Vitamin C helps your body produce the histamine-degrading enzyme, diamine oxidase (DAO).
And a low histamine Vitamin C can support the reduction of histamine-induced inflammation in the body. It’s also a rich antioxidant.
Anything that you can do to support lowering histamine will reduce mast cell activation.
And reducing mast cell activation means you aren’t getting a steady stream of that mast cell mediator, Elastase-2 in your system. This is the one that can contribute to breaking down connective tissue.
If you don’t have oxalate issues, you can consider up to 1000mg of Vitamin C 3x/day.
If you do have some oxalate issues, you may need to keep to 500 to1000mg daily.
With severe oxalates issues, consider even less at 250mg max per day.
Here is the Magnesium Ascorbate form that tends to be best tolerated by those with MCAS.
Aloe (Polysaccharides)
Aloe has been shown to help with immunoregulation. It’s also been shown to have these properties:
- Anti-cancer
- Anti-oxidation
- Wound healing
- Help repair connective tissue
- Neuroprotection
- Intestinal health
Since many types of EDS manifest with symptoms of slow wound healing, joint pain and degeneration, and intestinal issues, you can see where this supplement could be helpful.
You can consider starting with 1 to 2 teaspoons per day. As tolerated, you can consider working up to ¼ to 1 cup 2x per day.
And you’ll want to note that aloe can have laxative properties. So, if you are prone to diarrhea, you may want to start this one very slowly.
To keep your aloe low histamine, you’ll want to get it from a frozen source like Stockton Aloe.

Glucosamine Chondroitin
Glucosamine and chondroitin protect cells which help maintain cartilage structure.
Some people take these supplements to support joint health.
I’ve seen improvement for myself by taking this Glucosamine Chondroitin.
Isoquercitrin
Quercetin is one of my top recommendations for mast cell support. It can also help with histamine.
You might be getting some quercetin in your diet already. Do you eat a lot of brightly colored produce like apples and red cabbage?
These are great sources of quercetin. But you can support your mast cells even more with a supplement like isoquercitrin.
This Alpha-Glycosyl Isoquercitrin by Integrative Therapeutics is a form of quercetin that is more bioavailable than some other forms. That means your body can absorb it better and use it more efficiently.
Learn more about the benefits of quercetin here.
Vitamin D3 with K2
Remember that anything you can do to support mast cells will likely also help with EDS.
Vitamin D3 with K2 supports mast cells and GI (gastrointestinal) integrity.
Most mast cell experts recommend keeping D-25OH levels between 60 to 100.
You can work with your provider to test your levels about every 6 months to be sure you are on the right track.
Here is which vitamin D with K2 is most well tolerated.
If you are hypersensitive, you may want to try vitamin D without the K.
Click the link to learn more about Vitamin D and MCAS.
Magnesium
Recent data suggests that about 50% of the US population is magnesium deficient.
Part of the cause of this may be because the soil our food grows in has been depleted of a lot of natural minerals.
That’s why we often look to supplements to help support our health.
This can be especially valuable for those who are only tolerating a handful of foods.
Magnesium plays a lot of functions in the body. In regard to hEDS, magnesium may be helpful because it can assist with mast cell and histamine support. And it can help with muscle function.
You can learn more about the benefits of magnesium here. There are a lot of special considerations depending on your case.
Salt
Low blood pressure can be common with EDS. See, blood vessels are connective tissues. And EDS affects your connective tissues.
Weakened connective tissue can result in low blood pressure.
If you have low blood pressure, it’s important to keep your salt up. But it needs to be an unrefined sea salt like Redmond’s Real Salt.

Many people need 2000 to 5000mg per day. This is about 1 to 2 teaspoons or more per day.
You will likely get some salt from meals you prepare.
Just be sure that overall, you are getting enough salt.
This is why it’s so important to work with your provider. Track your blood pressure to make sure you don’t overshoot your intake.
Salt intake can also be an important part of keeping other electrolytes like magnesium and potassium in check.
CBD
With hEDS, you may be dealing with a lot of joint and muscle pain.
I was. That’s why I used the Kinesio tape so much.
Pain management is a big part of dealing with a lot of chronic illnesses like Mast Cell Activation Syndrome.
And it’s a big part of dealing with painful diseases that directly affect your joint and muscles.
One consideration for pain management is CBD (cannabidiol) which is derived from full spectrum hemp and non-hemp sources.
Here is the organic CBD that is generally well tolerated by those with MCAS.

Use coupon code MASTCELL360 for 20% off!
However, like any supplement, everyone’s tolerance is different. Work with your provider to find out what is best for you.
PEA (Palmitoylethanolamide)
If you haven’t tolerated CBD in the past, you may not tolerate PEA either.
Both use the same receptors in the brain.
But if you can tolerate it, PEA can be considered for pain management. It is also a cannabinoid. However, it is classified differently because your own body can make PEA.
PEA has been observed to have the following beneficial properties:
- Anti-inflammatory
- Antimicrobial
- Immunomodulatory
- Neuroprotective
Here is the PEA I recommend in the clinic.
EDS Aware Physical Therapy
Physical therapy is critical for hEDS.
It strengthens muscles to hold joints in place.
With EDS, your ligaments and tendons have lost integrity. So, you need to do what you can to rebuild your strength in your muscles.
There’s a book called Living Life to the Fullest with EDS. My physical therapist and I worked together to use this program as a basis for my physical therapy.

You may need to modify the program as well if you have MCAS and other sensitivities. However, it makes a good foundation for getting started.
Gentle Chiropractic Care
Chiropractic care can also be helpful. But you want a chiropractor with a clear understanding of EDS.
You don’t want to make matters worse by loosening joints too much.
An activator is preferred over manual manipulations. You may want to call ahead and ask if the chiropractor is familiar with this tool and EDS.
It is much gentler and easier on your body.
My physical therapist taught me to use an activator on my ribs myself. This really helped me with pain when I couldn’t get to my chiropractor. Here’s an activator similar to mine.

Prolotherapy (PRP or Dextrose)
This is something you’ll consider in the long term. You’ll want to consider prolotherapy only after MCAS and other triggers have been resolved.
Prolotherapy can regenerate the ligaments if they aren’t completely torn.
There are many types of prolotherapy.
You receive injections of substances like:
- Sugar
- Saline
- Platelet rich plasma (usually better tolerated because it’s from your own body)
- Ozone
These are meant to act as an irritant. Your body will then send immune cells to the area to help initiate a natural healing process.
This may sound a lot like mast cell activation to you. And it is. Remember, your mast cells are immune cells. They play an important role in healing and protecting you.
But that’s exactly why you want to have your MCAS under control before you consider prolotherapy.
And it’s very important to have an experienced provider.
There is no set standard of care right now. So, protocols are quite varied. You want someone who is well-versed in EDS. Preferably, they’ll have some knowledge of MCAS and sensitivities as well.
And I highly recommend having a flare plan in place to implement both before and after your sessions.
Please let me know your questions about flare plans in this week’s upcoming Facebook Live!
You don’t need a Facebook account to watch! Click the link or image above to get reminders and to watch live.
What to Avoid if You Have EDS
Sometimes, we think one thing is going to help. But it ends up making us feel worse. This happened to me with massage.
My whole body went into painful spasms after I had a massage on my abdominal muscles.
I later realized this was because ligaments along my spine had lost integrity and couldn’t hold me up.
Here are the top mistakes you might make with hEDS. You’ll want to avoid these.
- Massage – You need your muscles to hold your joints. Massage relaxes the muscles.
- Stretching – It can make matters worse by loosening joints and muscles.
- Collagen – It can generate oxalates, is a potential mast cell trigger, and is high histamine.
Here’s a little more on collagen.
Collagen gets broken down into individual amino acids. So, it’s just an amino acid replacement.
Instead of taking a collagen supplement, you can:
- Increase protein
- Support digestion to break down protein
- Add an amino acid supplement, if tolerated
How Am I Doing with MCAS and hEDS Now?
Now, I have to tell you that after getting EDS under control, it returned recently.
I had 2 bad mold exposures. And I underwent some medical treatments. Unfortunately, I didn’t follow my own advice! I didn’t put my flare plan into action before the treatments.
So, between the mold and the treatments, my MCAS flared out of control.
Something as simple as stubbing my big toe caused it to dislocate.
My skin is stretchy again.
And joints are subluxing easily.
But I’ve already started a protocol like what I shared with you above. I’ve come back from this before and I know I can do it again.
More than anything, that’s what I want to impart you with: hope.
We all have setbacks. But we can all make great strides forward, too.
I’ve been struggling with health issues almost my entire life. But hope has kept me going even in my darkest times.
I’ve learned that the cracks are where the light gets through. Don’t give up hope!
Do you suspect you have a type of EDS? Share your experience in the comments below!
Some links in this website are affiliate links, which means Mast Cell 360 may make a very small commission if you purchase through the link. It never costs you any more to purchase through the links, and we try to find the best deals we can. We only recommend products that we love and use personally or use in the Mast Cell 360 practice. Any commissions help support the newsletter, website, and ongoing research so Mast Cell 360 can continue to offer you free tips, recipes, and info. Thank you for your support!
References
Afrin, L. B., et al. (2020). Diagnosis of mast cell activation syndrome: a global “consensus-2”. Diagnosis (Berlin, Germany), 8(2), 137–152. https://doi.org/10.1515/dx-2020-0005
American Osteopathic Association. (2018, February 26). Low magnesium levels make vitamin D ineffective: Up to 50 percent of US population is magnesium deficient. ScienceDaily. Retrieved July 16, 2023 from www.sciencedaily.com/releases/2018/02/180226122548.htm
Assessing Joint Hypermobility – The Ehlers Danlos Society. (2023, May 3). The Ehlers Danlos Society. https://www.ehlers-danlos.com/assessing-joint-hypermobility/#1667832299890-fb92da86-9c8b
Bartonella home | CDC. (2022, January 12). Centers for Disease Control and Prevention. https://www.cdc.gov/bartonella/index.html
Beckstrand, R. L., PhD, RN, CCRN, CNE, & Pickens, J. S., BS, RN. (2011). Beneficial Effects of Magnesium Supplementation. Sage Journals, 16(3), 181–189. https://doi.org/10.1177/2156587211401746
Bowen, J. M., Sobey, G., Burrows, N., Colombi, M., Lavallee, M., Malfait, F., & Francomano, C. A. (2017). Ehlers-Danlos syndrome, classical type. American Journal of Medical Genetics Part C: Seminars in Medical Genetics, 175(1), 27–39. https://doi.org/10.1002/ajmg.c.31548
Chau, A. S., MD, MSE, & Jongco, A. M., MD, PhD, MPH, FAAAAI. (2018). Allergic and Immunologic Dysregulation in Ehlers-Danlos Syndrome: A Case Series. The Journal of Allergy and Clinical Immunology, 141(2), AB125. https://doi.org/10.1016/j.jaci.2017.12.398
DiNicolantonio, J. J., O’Keefe, J. H., & Wilson, W. (2018). Subclinical magnesium deficiency: a principal driver of cardiovascular disease and a public health crisis. Open heart, 5 (1), e000668. https://doi.org/10.1136/openhrt-2017-000668
EDS, POTS, Dysmotility, and Autoimmunity in MCAS (K. McCann, MD & B. O’Hara, FN, Guest and Interviewer). (2022). Reversing Mast Cell Activation And Histamine Intolerance Summit, United States of America. https://drtalks.com/videos/eds-pots-dysmotility-and-autoimmunity-in-mcas/
EDS Types – The Ehlers Danlos Society. (2023, January 11). The Ehlers Danlos Society. https://www.ehlers-danlos.com/eds-types/
Ehlers-Danlos Syndrome and MCAS Connection (A. Guggenheim ND & K. McCann MD, Guest and Interviewer). (2023). The Many Manifestations of Mast Cell Activation Summit, United States of America.
Glucosamine, chondroitin for osteoarthritis pain | Arthritis Foundation. (n.d.). https://www.arthritis.org/health-wellness/treatment/complementary-therapies/supplements-and-vitamins/glucosamine-chondroitin-osteoarthritis-pain
Islam, M., Chang, C., & Gershwin, M. E. (2020). Ehlers-Danlos Syndrome: Immunologic contrasts and connective tissue comparisons. Journal of translational autoimmunity, 4, 100077. https://doi.org/10.1016/j.jtauto.2020.100077
Kumar, B., & Lenert, P. (2017). Joint Hypermobility Syndrome: Recognizing a Commonly Overlooked Cause of Chronic Pain. The American journal of medicine, 130(6), 640–647. https://doi.org/10.1016/j.amjmed.2017.02.013
Liu, C., et al. (2019). Extraction, Purification, Structural Characteristics, Biological Activities and Pharmacological Applications of Acemannan, a Polysaccharide from Aloe vera: A Review. Molecules (Basel, Switzerland), 24(8), 1554. https://doi.org/10.3390/molecules24081554
Li, Y., et al. (2016). Quercetin, Inflammation and Immunity. Nutrients, 8(3), 167. https://doi.org/10.3390/nu8030167
Mozayeni, B. R., et al. (2018). Rheumatological presentation of Bartonella koehlerae and Bartonella henselae bacteremias: A case report. Medicine, 97(17), e0465. https://doi.org/10.1097/MD.0000000000010465
Nathan, N. (2018). Toxic. Victory Belt Publishing.
NHS. (2022, October 7). Ehlers-Danlos syndromes. nhs.uk. Retrieved July 14, 2023, from https://www.nhs.uk/conditions/ehlers-danlos-syndromes/
What is EDS? – The Ehlers Danlos Society. (2023, May 19). The Ehlers Danlos Society. https://www.ehlers-danlos.com/what-is-eds/



Thank you so much for the blog, I am learning a lot!!! Does pectus escavatum have something to do with ehlers danlons/hypermobility?
Hi Andreína! Yes, EDS can be a risk factor for pectus escavatum.
All my life I thought it was “Special” to be so double jointed…
I also was always sensitive to foods and hydrocarbons. I puked a lot. I had creamy skin that was frequently complimented.
When I turned 35 I started getting horrible headaches… Now I am 72 and thanks to you, I finally know what happened and am able to reclaim some of my life by avoiding triggers.
Thank you!!!
Hello,
My three year old just saw our DO because he’s overly flexible. It’s affecting his walking now. His DO referred him to our children’s hospital to see a physical therapist and a podiatrist. Are these supports listed in the article appropriate for kids?
Thank you!
Hi Rebecca, in regards to children, we always recommend discussing supplements and dosing questions with their pediatrician who is familiar with their case.