
What Are Oxalates? The MCAS and Oxalate Intolerance Connection
I’d never heard of Oxalate Intolerance or even oxalates when I was in my 20s.
So, I didn’t know that oxalates were part of the reason I was using a cane almost daily in my late 20s.
What I did know is I was embarrassed using a cane out in public. I’d see the questioning looks people gave me.
I guess it seemed strange to them that I was so young and needed a cane. I even had people tell me I didn’t look sick.
But the truth is, I should have been in a wheelchair. That’s how bad my health issues were.
My knees felt like they had ground glass inside them most days.
It would take me 5 minutes to walk somewhere that took my husband only 30 seconds.
Have you struggled just to get to your car so you could drive to the doctor?
Or has grocery shopping become so painful you do all your shopping online now?
Have you had to miss special celebrations because your body hurt so badly?
And amid all your pain, has someone said you look “normal” so you can’t possibly be that sick?
I’ve been there.
But here’s the good news. I haven’t needed a cane for years.
I feel good enough to walk in the woods every week. I can even hike and scuba dive on vacations again.
What changed for me?
Keep reading to find out more about how Oxalate Intolerance was affecting me and how it might be affecting you, too.
You’ll learn more on:
- What is Oxalate Intolerance?
- What are oxalates?
- Symptoms of Oxalate Intolerance
- What Contributes to Oxalate Intolerance?
- Oxalates and inflammation
- The connection between Oxalate Intolerance and Mast Cell Activation Syndrome
- Testing for Oxalate Intolerance
So just what are oxalates and where do they come from?
What Are Oxalates?
It’s important you know that this blog post is for informational and educational purposes. It’s not meant to treat any health condition or to be prescriptive for anyone. If you have any medical condition, it is critical you work under the care and guidance of a licensed medical provider.
Oxalic acid is an organic compound found in many plants.
Oxalic acid binds to minerals which then produces oxalates. For example, when oxalic acid binds to calcium, calcium oxalate is produced. (This is what can lead to calcium oxalate kidney stones.)
There are different types of oxalates based on what mineral the oxalic acid binds to.
Though oxalic acid and oxalates are technically two different things, you’ll often see these terms used interchangeably in common language.
So, what are oxalates and why do you need to know about them?
Where Oxalates Come From
Oxalates are part of a plant’s defense mechanism. When you eat certain plants, you ingest these oxalates.
Under a microscope, oxalates look like tiny shards of glass or little razor blades.
Oxalates protect plants from viruses and bacteria.
They’re also meant to deter insects and grazing animals. (Doesn’t that make you wonder if you should be eating plants with high amounts of oxalate?)
Certain plant foods have particularly high concentrations of oxalic acid.
Some of the highest oxalate plant foods are:
- Fruits – kiwi, blackberries, pomegranates, plantains
- Vegetables – beets, rhubarb, sweet potatoes, okra, Swiss chard, spinach
- Grains – buckwheat, brown rice, oats
- Legumes – kidney beans, lentils, soybeans, peanuts
- Nuts – cashews, almonds
- Seeds – sesame seeds (and tahini), pine nuts
- Other – chocolate
Many plants with high oxalate content are packed with antioxidants, vitamins, and minerals.
But unfortunately, oxalates act as an “antinutrient”.
Antinutrients are plant compounds that keep your body from absorbing those essential nutrients.
So, if you aren’t getting the right balance of foods, oxalates may be contributing to nutrient deficiencies.
And these high levels of oxalates may cause painful symptoms and conditions, too.
Related Article: Low Histamine Food List (with low oxalate foods!)
Let’s look at some potential problems of oxalates next.
What Is Oxalate Intolerance?
Some people don’t have problems with oxalates.
But for others, oxalates are extremely problematic.
Think of it like this.
What if you stepped on 1 thorn? It would hurt. But you could easily remove 1 thorn and carry on.
But what if you stepped on 100 thorns every day for a week? And what if you couldn’t remove them? That would take a toll on you!
That’s basically what Oxalate Intolerance is. Oxalate Intolerance is what happens when the amount of oxalate present is too much for your body to handle.
And among other problems, high levels of oxalate can leave you literally feeling like you’ve stepped on 100 thorns!
One of the biggest problems I had from oxalates was joint and muscle pain.
But for years, I didn’t know oxalates were partially responsible.
I went through a big guessing game figuring out what was causing my debilitating pain.
One chiropractor thought I had scar tissue. He tried a type of physical therapy that uses metal rods to try to mobilize scar tissue. It was torture.
The orthopedist couldn’t find any evidence of injury. So, he wanted to do exploratory surgery. I’m so glad I said no to that!
The rheumatologist thought I had an unusual form of rheumatoid arthritis that comes and goes. He gave me medications that he thought would help.
My general practitioner checked my blood work but didn’t see any autoimmune markers.
Everyone was guessing. And nothing helped because I wasn’t addressing the root problem. And one of my root problems was oxalates.
Next, take a look at some of the other symptoms in addition to joint and muscle pain that oxalates can cause.
Symptoms of Oxalate Intolerance
Before you change your diet on your own, make sure you’re working with a healthcare practitioner who can help you with this. Never limit foods unnecessarily, and always have a licensed medical provider who is supervising your case.
When your body can’t manage your oxalate load, you can end up with Oxalate Intolerance.
Your body becomes hyper-sensitive to oxalates and can’t tolerate them anymore.
That’s why you may have reactions when you eat high oxalate foods.
And that’s why eating a low oxalate diet can help.
IMPORTANT: DO NOT go low oxalate cold turkey! This can make you very sick. Learn more about oxalate dumping here.
Food intolerance is not the only issue you can get from oxalates.
Here are some of the known problems oxalates have been associated with:
- Asthma
- Arthritis
- Autism
- Autoimmunity
- Back pain
- Breast Cancer
- Burning mouth
- Candida overgrowth
- Cardiovascular disease
- Cataracts
- Cellular damage
- Chronic infections
- Diverticulosis / Diverticulitis
- Ear crystals
- Electrolyte deficiencies
- Endometriosis
- Eye pain and burning
- Fatigue
- Fibromyalgia
- Hair loss
- Hemorrhoids
- IBD (Irritable Bowel Disease)
- IBS (Irritable Bowel Syndrome)
- Inflammation (or worsen existing inflammation)
- Interstitial Cystitis (urinary burning and pain similar to urinary tract infections)
- Joint and muscle pain
- Kidney stones
- Leaky gut
- Mast Cell Activation Syndrome
- Migraines
- Mineral deficiencies
- Neurological symptoms
- Nutrient deficiencies
- Osteoporosis and Osteopenia
- Polycystic Ovary Syndrome (PCOS)
- Pulmonary Fibrosis
- Reflux
- Refractory anemia
- Reynaud’s (often characterized by cold hands and feet)
- Sandy eye excretions
- Sandy stools
- Sleep disorders
- Thyroid dysfunction
- Tooth or bone pain
- Tissue damage
- Uterine fibroids
- Vascular damage
- Vertigo
- Vulvodynia
- White spots on skin
It’s important to mention that any of these conditions may be caused by something other than oxalates, too. That’s why it’s so important to work with your provider.
Eventually I learned oxalates lodge in various tissues throughout the body. Like muscles, joints, and eyes.
My fibromyalgia, joint pain, and urinary pain all stemmed from oxalates. When I balanced my oxalates, these all went away.
So, what’s contributing to your oxalate load?
Find out next.
What Contributes to Your Oxalate Load?
You’ve read about how high oxalate intake from plant foods may be one way you are getting oxalates.
But that’s not the only thing that may be contributing to high oxalate levels.
Here are a few reasons why you may be struggling with oxalates.
Mold Colonization
Mold Colonization can contribute to your oxalate load.
With Mold Colonization, mold is growing in your body.
Typically, this starts by breathing in mold spores. This can happen when you have a lot of ongoing exposure to mold.
Once you breathe in mold spores, they can end up anywhere in your body. And they can take hold.
Some people can fight off these mold spores. But other people can’t and end up with Mold Colonization.
If you do have Mold Colonization, certain molds can make oxalates.
One type is aspergillus.
Did you know? Candida feeds on oxalates? That means a high oxalate diet may be contributing to candida issues. Oxalates may be a food source for other fungal species as well.
Learn more about MCAS and Candida here.
For more on Oxalates and Mold, check out this video.
Note: you do not need a Facebook account to watch.
Leaky Gut
Leaky gut is an intestinal issue.
Leaky gut happens when the lining of the intestinal wall is compromised. This allows particles like oxalates to enter the blood stream.
Your body will view these oxalates as toxic. And it will want to prevent them from being circulated in your body. So, your body will store oxalates in your tissues where they are “out of circulation”.
That doesn’t mean they won’t cause problems, though.
Depending on which tissues these oxalates get stored in can influence the kinds of symptoms you will have.
Oxalates can also cause leaky gut. So, oxalates can be part of a vicious cycle here. They can cause leaky gut. And leaky gut can lead to circulation of oxalates contributing to your oxalate load.
Dysbiosis
Dysbiosis is another gut issue. It happens when your gut microbiome is out of balance.
That just means that the flora-like bacteria and even good fungi are off kilter in your gut.
This can interfere with the body’s ability to excrete oxalates.
That’s because some of the natural bacteria in your gut will break down dietary oxalates.
Both leaky gut and dysbiosis can lead to higher levels of oxalates in your body.
Learn more about gut health in this related article: Enzymes, Short-Chain Fatty Acids (SCFA’s), and Gut Health in SIBO, Mast Cell Activation Syndrome, and Histamine Intolerance
Glyphosate Exposure
Glyphosate is the active ingredient in pesticides like the weedkiller, Roundup.
If the detox pathway that metabolizes glyphosate becomes overwhelmed, your body can create more oxalate.
Nowadays, we are exposed to so much glyphosate through conventional produce and our environment that it’s no wonder I see so many clients with extremely high levels of glyphosate.
Oxalate Genetic Variants
I like to remind people that genetics aren’t necessarily a life sentence. For most people, it’s genetic expression that plays a bigger role.
But genetics can make you more susceptible to certain things if conditions are right.
For example, you may have certain genetic variants that make you more susceptible to higher oxalate levels based on how your body can metabolize them.
For example, you could have genetic variants for low B1 or B6. Let’s look more at the role B1 and B6 play in oxalates next.
Low B1 or B6
People who have low B1 or B6 may produce more oxalates than those who don’t. See, oxalates don’t just come from outside sources like food. Your body makes them, too.
B vitamins play a role in metabolizing oxalates in your body.
So, if you don’t have enough B1 or B6, you could end up with higher concentrations of oxalates.
Did You Know? B1 is easily depleted by high carb diets and mycotoxins (toxins from mold)?
Low Sulfate
Sulfur plays a role in metabolizing food.
You can get sulfur in your diet from sulfur rich foods like broccoli and cauliflower.
But you might be eating low FODMAP due to FODMAP issues, for example.
In which case, your sulfur may be low.
And low sulfur can contribute to impaired metabolization of foods containing oxalates.
Related Article: FODMAP Intolerance: What to Know if You Have Mast Cell Activation Syndrome or Histamine Intolerance
High Vitamin C Consumption
Generally speaking, vitamin C is a plus if you have Histamine Intolerance or MCAS.
Learn more about Low Histamine Sources of Vitamin C in this post.
However, in some cases, very high concentrations of vitamin C can add to your oxalate load.
That’s because vitamin C, either from foods or supplements, can be converted into oxalates.
Normally this is excreted in your urine, though. However, if you are taking a lot of vitamin c, the oxalates produced may be too much for normal excretion.
Now you know why oxalate levels may be high for you.
And you know that this may lead to food intolerances.
You’ve also read that oxalates have been associated with a lot of different symptoms and conditions. Including Mast Cell Activation Syndrome and Histamine Intolerance.
Let’s explore that connection more next. Then I’ll tell you how to test to see if oxalates may be a problem for you.
Oxalates, Mast Cell Activation Syndrome, and Histamine Intolerance
Many people who think they just have Histamine Intolerance actually have much more going on. Including oxalate issues.
Remember when we talked before about oxalates being like microscopic razor blades or crystals of glass?
Those sharp, microscopic crystals scrape tissues and can cause tissue damage. Mast cells go into action to start the healing process any time there is tissue damage.
But, if you have Mast Cell Activation Syndrome, this process can get out of control.
The mast cells will release histamine and numerous other inflammatory mediators. This can worsen Histamine Intolerance, too.
So, how can you know if you have oxalate issues yourself?
There are 3 things that need to be looked at:
- Symptoms
- Oxalate lab markers
- Genetics
Earlier you read about some of the common symptoms related to oxalates.
Next, learn more about the other 2 important aspects – lab markers and genetics.
Testing for Oxalates
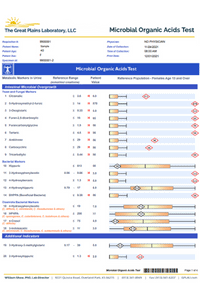
The best test to look at oxalate issues is the Great Plains Organic Acid Test. This is an at-home urine test.
This panel looks at areas including:
- 3 different types of oxalate markers
- Gut markers for fungal and bacterial overgrowth
- Metabolism markers for fats, carbs, and proteins
- Detoxification markers
- Nutrient markers
- Ammonia levels
The best part is you can order it for yourself here:
>>> Great Plains (now Moasaic DX) Organic Acid Test with Oxalate Markers
Here is the link for those in Canada:
>>> CANADA Great Plains Organic Acid Test
(Private clients: You have gotten this test already or will get it soon, so let us handle it from the office for you. This link is for those who don’t have an appointment.)
You can learn a lot from taking this test.
But today, we’ll just look at a brief overview of the oxalate markers.
Oxalate Markers
There are 3 oxalate markers on the Great Plains Organic Acid Test.
These show levels of:
- Oxalic – This marker gets elevated from a few different causes including:
- Mold Toxicity
- Leaky gut
- Eating a lot of high oxalate foods
- Antibiotic overuse
- High doses of Vitamin C
- Genetic issues
- Glyceric – This marker can be elevated from:
- Genetic issues with GRHPR (more below)
- Lack of B6 and B1
- Glycolic – This marker can be elevated from:
- Genetic issue with AGXT (more below)
- Lack of B6 and B1
Here’s what you need to know about testing.
Remember when you read that your body can store oxalates in tissues to keep them from circulating throughout your body?
That means sometimes the oxalic marker can show in range even when there are oxalate issues. This is because it is stuck in the joints, muscles, etc. and isn’t showing in excretion of urine.
This is why we want to always pay attention to symptoms and genetics in addition to test markers.
Speaking of genetics. Let’s look at that next.
Genetics Related to Oxalates
There are 4 enzymes and genes to look at in relationship to oxalates and the markers above.
These are:
- GRHPR
- SPP1
- HOGA1
- AGXT
So, what do these genes and enzymes do?
In general, all of them in one way or another reduce the buildup of oxalates in the body.
But if these enzymes aren’t working correctly, you can get an increase in glyceric or glycolic acids.
These enzymes can be affected by:
- Oxalate genetic variants
- Lack of B1 or B6
- Glyphosate
- Low sulfates (from avoiding sulfate foods)
Now you know:
- What oxalates are
- Problems oxalates can cause
- How to test for high levels of oxalates
Learn more about your oxalate levels with the Great Plains Labs (now Mosaic DX) Organic Acids Test.
>>> US residents order your Great Plains Labs (now Mosaic DX) Organic Acids Test here!
If you’re in Canada, you can order the Great Plains Labs (now Mosaic DX) Organic Acid Test here.
Oxalate dumping can happen if you reduce your intake of oxalates too quickly.
If you have high levels of oxalates, you’ll want to work on reducing them gradually.
Do not quit oxalates cold turkey. You must reduce them slowly. You can end up feeling really miserable if you don’t.
So, keep an eye out for that blog post next to learn how to handle oxalates so you don’t end up feeling sicker.
Beyond Oxalate Intolerance
Some links in this website are affiliate links, which means Mast Cell 360 may make a very small commission if you purchase through the link. It never costs you any more to purchase through the links, and we try to find the best deals we can. We only recommend products that we love and use personally or use in the Mast Cell 360 practice. Any commissions help support the newsletter, website, and ongoing research so Mast Cell 360 can continue to offer you free tips, recipes, and info. Thank you for your support!
References
Special thanks to Emily Givler, Monique Attinger, and Susan Owens for their work in the area of oxalates. Much of what I’ve learned about oxalates, I’ve learned from them and have customized for those with Mast Cell Activation and Histamine Intolerance.
Barr-Beare E, et al. (2015) The Interaction between Enterobacteriaceae and Calcium Oxalate Deposits. PLOS ONE 10(10): e0139575. https://doi.org/10.1371/journal.pone.0139575
Brzica, H., et al. (2013). Oxalate: from the environment to kidney stones. Arhiv za higijenu rada i toksikologiju, 64(4), 609–630. https://doi.org/10.2478/10004-1254-64-2013-2428
Castellaro, A. M., Tonda, A., Cejas, H. H., Ferreyra, H., Caputto, B. L., Pucci, O. A., & Gil, G. A. (2015). Oxalate induces breast cancer. BMC cancer, 15, 761. https://doi.org/10.1186/s12885-015-1747-2
Chai, W., Liebman, M., Kynast-Gales, S., & Massey, L. (2004). Oxalate absorption and endogenous oxalate synthesis from ascorbate in calcium oxalate stone formers and non-stone formers. American journal of kidney diseases : the official journal of the National Kidney Foundation, 44(6), 1060–1069. https://doi.org/10.1053/j.ajkd.2004.08.028
Furuta, M., & Ozaki, M. (1970). Calcium oxalate crystals in the kidney and thyroid of leprosy patients. International Journal of Leprosy and Other Mycobacterial Diseases, 38(3), 286–293. http://ijl.ilsl.br/detalhe_artigo.php?id=MzM5OQ%3D%3D&secao=ORIGINAL+ARTICLE#
Ghio, A. J., Roggli, V. L., Kennedy, T. P., & Piantadosi, C. A. (2000). Calcium oxalate and iron accumulation in sarcoidosis. Sarcoidosis, vasculitis, and diffuse lung diseases : official journal of WASOG, 17(2), 140–150.
Givler, Emily. Lecture on Oxalates. Environmental Toxins and Genomics Conference. 2019.
Goldman, M., & Doering, G. J. (1979). The effect of dietary ingestion of oxalic acid on thyroid function in male and female Long-Evans rats. Toxicology and applied pharmacology, 48(3), 409–414. https://doi.org/10.1016/0041-008x(79)90424-1
Hackett, R. L., & Khan, S. R. (1988). Presence of calcium oxalate crystals in the mammalian thyroid gland. Scanning microscopy, 2(1), 241–246.
Katoh, R., et al. (1993). Birefringent (calcium oxalate) crystals in thyroid diseases. A clinicopathological study with possible implications for differential diagnosis. The American journal of surgical pathology, 17(7), 698–705. https://doi.org/10.1097/00000478-199307000-00007
Katoh, R., et al. (1993). Nature and significance of calcium oxalate crystals in normal human thyroid gland. A clinicopathological and immunohistochemical study. Virchows Archiv. A, Pathological anatomy and histopathology, 422(4), 301–306. https://doi.org/10.1007/BF01608339
Mahapatra, T. P., et al. (1986). Vesical calculi associated with vesicovaginal fistulas: management considerations. The Journal of urology, 136(1), 94–95. https://doi.org/10.1016/s0022-5347(17)44742-2
Muntz F. H. (1999). Oxalate-producing pulmonary aspergillosis in an alpaca. Veterinary pathology, 36(6), 631–632. https://doi.org/10.1354/vp.36-6-631
Norton, S.K. (2022). Toxic Superfoods: How Oxalate Overload Is Making You Sick–and How to Get Better. Rodale Books. https://amzn.to/3CfQjGj
Pusztaszeri M. (2016). Birefringent crystals in thyroid fine-needle aspiration cytology. Diagnostic cytopathology, 44(10), 814–815. https://doi.org/10.1002/dc.23562
Reid, J. D., Choi, C. H., & Oldroyd, N. O. (1987). Calcium oxalate crystals in the thyroid. Their identification, prevalence, origin, and possible significance. American journal of clinical pathology, 87(4), 443–454. https://doi.org/10.1093/ajcp/87.4.443
Reid J. D. (1991). Calcium oxalate in mammalian thyroids: a re-evaluation. Journal of comparative pathology, 105(1), 109–115. https://doi.org/10.1016/s0021-9975(08)80066-7
Sarraf, P., Kay, J., & Reginato, A. M. (2008). Non-crystalline and crystalline rheumatic disorders in chronic kidney disease. Current rheumatology reports, 10(3), 235–248. https://doi.org/10.1007/s11926-008-0038-1
Sarma, A. V., et al. (1999). Epidemiology of vulvar vestibulitis syndrome: an exploratory case-control study. Sexually transmitted infections, 75(5), 320–326. https://doi.org/10.1136/sti.75.5.320
Shimizu, M., et al. (1999). Calcium oxalate crystals in thyroid fine needle aspiration cytology. Acta cytologica, 43(4), 575–578. https://doi.org/10.1159/000331148
Verbruggen, L. A., Bourgain, C., & Verbeelen, D. (1989). Late presentation and microcrystalline arthropathy in primary hyperoxaluria. Clinical and experimental rheumatology, 7(6), 631–633.
Wahl, R., Fuchs, R., & Kallee, E. (1993). Oxalate in the human thyroid gland. European journal of clinical chemistry and clinical biochemistry : journal of the Forum of European Clinical Chemistry Societies, 31(9), 559–565. https://doi.org/10.1515/cclm.1993.31.9.559
Wigner, P., Bijak, M., & Saluk-Bijak, J. (2022). Probiotics in the Prevention of the Calcium Oxalate Urolithiasis. Cells, 11(2), 284. https://doi.org/10.3390/cells11020284
Zimmerman, L. E., & Johnson, F. B. (1958). Calcium oxalate crystals within ocular tissues; a clinicopathologic and histochemical study. A.M.A. archives of ophthalmology, 60(3), 372–383. https://doi.org/10.1001/archopht.1958.00940080388005




What do you do if you live in NY where it’s illegal to collect or ship the test?
Is there another way, such as an elimination diet?
Hi Beth,
The labs can’t legally ship to NY and collection can’t be done in NY.
Most people in NY have these types of tests shipped to a relative or friend in a neighboring state, collect while out of state, use the friend/family member’s address, and mail the test back from out of state.
Hello! I am very interested in pursuing this for my mast cell issues. Upon beginning the elimination diet, how does one go about determining what to avoid: histamine or oxalates? As avoiding both would be very restrictive.
Thank you!
Hi Mabel, I would start with eliminating histamines if you are unsure. Quitting oxalates cold turkey isn’t the best course of action. I hope you will be able to join my upcoming Facebook Live on Monday June 22, 2020 when I talk about what to do for reducing oxalates from your diet. Also, please take a look at my most current blog post to find out more about addressing oxalate issues. You can find that here: https://mastcell360.com/oxalates-part-ii-addressing-when-you-have-mast-cell-activation-syndrome-and-histamine-intolerance/ Thanks!
I use mast360 and an an app that helps me chose low histamine foods. Is there a list of food that shows me what had oxylates in them? This sounds like my problem.
Hi Heather,
This list show oxalates with the letter O next to the food:
https://mastcell360.com/low-histamine-foods-list/
Suz
Hi Beth,
Is celery juice a high oxalate option? I’m getting mixed reviews.
Thanks,
Leah
Hi Leah,
A 1/2 cup serving of raw celery juice is medium oxalate.
Best,
Jamie
Are artichokes and hearts of palm high oxalate?
Hi Che,
In testing, one medium-sized, boiled artichoke had about 8 grams of oxalates, making it a medium oxalate food. While a 1/2 cup serving of boiled artichoke hearts contains about 28 grams! That makes the hearts very high. Just like histamines though, it’s a bucket with a cumulative total and the objective is to keep it under our personal limit. Those limits vary by person and sometimes day to day.
-Kam
I’d really like to watch your video, but 58 min. of people speaking slowly takes far too much time out of my life. Especially when whole segments of that is chitchat. Why do so many podcasters do that? Please consider putting your videos on Youtube or some other platform where your listeners can change the speed, or allow listeners to download. And perhaps consider making chapters so listeners can skip to the relevant segments that are pertinent to them.
Hi Jan, thanks so much for the feedback. We do have a YouTube channel, and are working on moving previously recorded videos over to this platform. While not all are up there yet, you may find some of interest that you can explore here: https://www.youtube.com/@mastcell360