
MCAS Symptoms: Debunking Myths About Mast Cell Activation Syndrome and Histamine Intolerance
Are you trying to figure out if your reactions are Mast Cell Activation Syndrome? Are you unsure about what the symptoms of Mast Cell Activation Syndrome or Histamine Intolerance really are?
Do you find yourself confused by all the different articles you see online?
I felt the same way once, too.
When I was first learning about Mast Cell Activation Syndrome (MCAS) and Histamine Intolerance, there was a lot of misinformation out there.
I’m glad that more professionals are aware of these issues now. And I’m so glad they are talking about it and learning more every day.
But I still see misinformation about symptoms of Mast Cell Activation Syndrome all over the place.
I come across all kinds of myths like this one:
Myth #1: It Isn’t Possible to Heal from Mast Cell Activation Syndrome and Histamine Intolerance
That’s the #1 myth I don’t want you to believe!
Believing that and other myths can get in the way of your healing.
I’ve reclaimed my health from both Mast Cell Activation Syndrome and Histamine Intolerance.
So, how can you figure out what’s true and what’s false so you can start addressing symptoms?
Keep reading to learn more about common myths. But first, you may be wondering if you even have Mast Cell Activation Syndrome (MCAS).
Let’s talk a little about that next.
Mast Cell Activation Syndrome Symptoms
It’s important you know that this blog post is for informational and educational purposes. It’s not meant to treat any health condition or to be prescriptive for anyone. If you have any medical condition, it is critical you work under the care and guidance of a licensed medical provider.
Mast Cell Activation Syndrome symptoms can show up in almost any part of the body.
Do you have symptoms that you don’t really have an explanation for?
You’ll sometimes hear these referred to as “mystery symptoms.”
That’s because your bloodwork might look normal. And you may even hear annoying statements like, “You don’t look ill.”
But just because you “look fine” and have normal bloodwork doesn’t mean there isn’t something wrong. I think deep down, people looking for answers already know that. No matter what anyone may have told you otherwise.
That’s why I want you to know just how extensive Mast Cell Activation Syndrome symptoms can be. We’ll go over all of those in detail.
For now, I want you to know there are many! They can affect nearly any system in your body. And they may seem unrelated.
Before we discuss all of that I want to share some myths with you.
That’s because if you believe some of these myths, you may dismiss MCAS as a possibility, even if you have numerous symptoms.
I did.
I didn’t think it was my problem. I’d heard it was rare.
So, let’s start there.
Myth# 2: Mast Cell Activation Disorders are Rare
One of the first steps in my healing was learning that I had Histamine Intolerance.
I didn’t know I had Mast Cell Activation Syndrome (MCAS), too.
But while I was learning about Histamine Intolerance, I came across articles about Mast Cell Activation Syndrome. It sure seemed like that might be what was happening for me!
But I thought MCAS was rare. So, I didn’t explore it fully.
After all, if it was rare, then it wasn’t likely my problem. I was very wrong about that!
Eventually, I learned that sometimes Mast Cell Activation Syndrome is confused with Mastocytosis.
Mastocytosis is rare. It’s a mast cell activation disease in which there is an increased number of mast cells. You may also hear this called Systemic Mastocytosis.
Mast Cell Activation Syndrome is different. That happens when you have a normal amount of mast cells, but they are over-responsive.
That being said, some genetic forms of Mast Cell Activation Syndrome are rare. You’ll see this called clonal MCAS.
But the majority of Mast Cell Activation Syndrome is what is called non-clonal. This means it’s not related to the mast cell genes.
And non-clonal MCAS isn’t rare at all.
According to leading Mast Cell Disorder experts, including Dr. Lawrence Afrin, MCAS may be as common as 17% of the general population.
So, MCAS is more common than originally thought.
And all those symptoms you don’t have an explanation for may be MCAS symptoms!
Myth #3: The Major Trigger for Mast Cell Activation Syndrome Is Histamine
Some people only have Histamine Intolerance.
Some people only have Mast Cell Activation Syndrome.
However, in the Mast Cell 360 practice, we see many people with both.
Related Post: Do You Have One or Both? Histamine Intolerance vs MCAS
They can go hand in hand because histamine is a mast cell trigger. And when mast cells are triggered, they release histamine.
It’s a self-feeding cycle that can result in you feeling very sick.
But histamine is just one of many mediators released by mast cells.
There are over 1000 mediators! And many (but not all) of these mediators released by mast cells also trigger mast cell activation.
So, histamine alone isn’t the only mediator responsible for mast cell activation.
These mediators can also be triggers:
- Prostoglandins
- Tryptase
- Inflammatory leukotrienes
- Cytokines
- Interleukins
And mediators in general are just one of many possible reasons for activated mast cells.
It turns out that there are a lot of root causes for Mast Cell Activation Syndrome.
Root Causes of Mast Cell Activation Syndrome
Root causes are the big, underlying factors that contribute to your mast cell activation.
Many people have been told their MCAS is idiopathic. This means the cause isn’t known.
But today, we’re very clear that some of the biggest root causes of MCAS are:
- Mold Toxicity
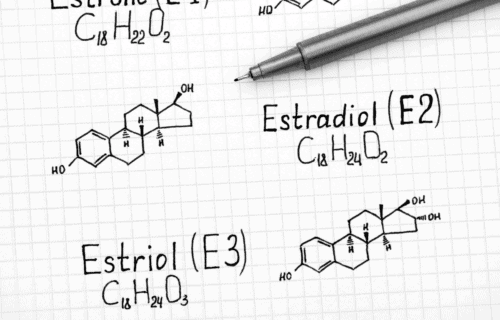
- Hormonal imbalances
- Infections
- Injuries, like concussions
- Genetic factors
- Nutritional deficiencies
- Stress and/or early trauma
- Food Triggers
- Histamine
- Oxalates
- Lectins
- Salicylates
- Glutamates
- FODMAPs
Do you have trouble with any of those underlying triggers?
Myth #4: Diet Changes Can’t Help Symptoms of Mast Cell Activation Syndrome
Before you change your diet on your own, please make sure you’re working with a healthcare practitioner who can help you with this. Never limit foods unnecessarily, and always have a licensed medical provider who is supervising your case.
If you’ve made changes in your diet and felt better, you already know this myth isn’t true either.
I started eating low histamine to help with Histamine Intolerance.
For a while, I didn’t know this was also helping my mast cell activation. (Like I said, for some time, I didn’t even know I had MCAS!)
But here’s how it helped.
Histamine can trigger mast cells. Then mast cells release more histamine. That triggers more mast cell activation. It can spiral out of control.
By eating low histamine, I was calming some of my mast cell response.
Eating low histamine helped me get on the right path toward wellness. But this alone didn’t do everything to address my MCAS symptoms.
In the section above, you just read that other inflammatory foods can be triggers, too.
This was definitely the case for me.
Have you tried the low histamine diet?
Did you get some relief, but are still dealing with symptoms?
If so, it may be helpful to explore what food sensitivities you may have. Eating to support your body can make a huge difference.
Mast Cell Activation Food Triggers
If you aren’t eating low histamine yet and want to learn more, check out the low histamine food list.
You’ll see a list of low histamine foods you can choose from.
And you’ll find higher histamine and histamine liberating foods listed, too. Those are the ones you’ll initially want to avoid if you have Histamine Intolerance.
But there are many food triggers that may be affecting you. Here are some of the more common ones.
- High histamine foods
- Wheat
- Dairy
- Corn
- Soy
- Sugar
- Processed foods and food additives
- Preservatives
- Oxalates
- Lectins (found in most grains, nightshades, grain-fed meat)
- FODMAPs
- Salicylates
- Glutamates
Not sure what your triggers are? Try keeping a food diary.
Simply write down the foods you eat and any reactions.
But keep this in mind:
- Some people have immediate reactions. This makes it fairly easy to sort out what is causing symptoms.
- Others won’t see reactions for a couple days. If that’s you, it’s extra important to work with a professional.
I had numerous food sensitivities.
It took some time before I got everything figured out. But once I did, I started seeing even more improvements.
But don’t cut out everything at once.
Work with your provider to figure out what is right for you.
And remember, food changes aren’t meant to be forever. Ideally, you’ll be able to start reintroducing a wider range of whole, nutrient dense foods again.
I have improved dramatically through changing my diet. I’ve seen many others make big strides toward healing by altering their diet, too!
Diet can help with Mast Cell Activation Syndrome.
Myth #5: There Is Nothing You Can Do About Genetics
Think of your genetics as the blueprint for your body.
And think of genetic expression like the builder who uses those blueprints to construct a building.
It’s really the builder (genetic expression) that will determine the building’s outcome.
Here’s how.
If there are mistakes (genetic variants) in the blueprint (the DNA), the builder may build according to the plans. In other words, mistakes in the blueprints will show up in the construction.
But what if the builder catches those mistakes before construction begins? She will correct for those.
On the other hand, what if the builder isn’t having a good day? She may not catch the original mistakes. And she may make her own mistakes, too!
As you can see, it’s not just those original blueprints that determine the outcome of the building.
So, what are those things that make the builder have a bad day? In other words, what are the things affecting your genetic expression?
These factors can all worsen your genetic expression:
- Mold toxins (mycotoxins)
- Chemical toxins
- Pathogens
- Stress
But if you address those factors, it’s amazing how much your genetic expression can repair!
Genetic Factors to Consider with MCAS or Histamine Intolerance
Genetics aren’t a life sentence.
I often hear statements like:
“I have an MTHFR variant so I can’t detoxify.”
Or, “I have a CBS variant so I can’t have anything with sulfur.”
Now, it’s true these genetic predispositions can significantly affect you when you have a lot of toxins, pathogens, and stressors.
As you just read, those are factors that affect your genetic expression.
But once those triggers are removed, your genetic expression can improve dramatically.
They can improve so much that many of your genetic variants may no longer be an issue.
This happened for me. And it can happen for you.
Knowing your genes allows you to work with your genetic expression. In other words, understanding your blueprints can help you construct a better building.
That’s where genetic testing and analysis can be beneficial.
In fact, I think it’s so important that I got certified in Functional Genomic Analysis to better help my clients!
If you like to learn through listening or watching be sure to check out my presentation on Debunking MCAS Myths.
Note, there’s no need for a Facebook account to watch!
Myth #6 Elevated Tryptase Levels Always Show Up in Testing for Mast Cell Activation Syndrome
Getting an official diagnosis of Mast Cell Activation Syndrome can be challenging.
Unfortunately, the testing markers used in the diagnosis are still quite problematic. From what I see, they only seem to capture about 10% of cases.
Diagnostic criteria are still being debated by researchers.
On one side of the fence, some experts say that tryptase is the only reliable marker for MCAS.
However, according to the more widely accepted “Consensus-2” criteria, there are a number of urine and blood tests for mast cell mediators that can be used in diagnosing Mast Cell Activation Syndrome (MCAS).
According to the Consensus-2 criteria, an elevation in any of these diagnostic markers can indicate MCAS.
Blood tests:
- Tryptase
- Chromogranin A
- Prostaglandin D2
- Histamine
- Heparin
Urine tests:
- Prostaglandin D2
- 2,3-Dinor-11beta-prostaglandin F2 alpha
- Histamine
- N-methyl histamine
- Leukotriene E4
There are still some challenges with this broader testing criteria though.
Challenges with Testing for MCAS
One very basic testing challenge is that urine or blood samples need to be kept chilled from the time of collection through processing.
Then, the lab must use a cold centrifuge. Yet very few labs have this equipment. This is leading to many of the false negative results.
Another challenge is getting an accurate reading to begin with. See, mast cell mediators in blood and urine can be elevated and then fall again very quickly.
But mediator levels can change rapidly. Even within a few minutes. This makes it sometimes very hard to catch them.
Mediators are chemicals mast cells release when activated.
If MCAS is suspected, some practitioners will try to provoke a flare and retest hourly for several hours in hopes of getting positive lab markers.
But even so, due to how fast these levels can rise and fall, you still may not get an accurate picture.
And speaking of mediators, that leads us to our myth – elevated tryptase levels always show up in MCAS tests.
Tryptase and MCAS Testing
Tryptase is one mediator released by mast cells.
If you’ve read up on MCAS testing, you may have heard that tryptase levels are always elevated in MCAS tests.
But according to the “Consensus-2” experts, tryptase is rarely elevated in MCAS.
Tryptase is more commonly a marker for Mastocytosis and Hereditary Alpha Tryptasemia (a genetic disorder that can be associated with Mastocytosis.)
Many providers are no longer looking for elevated tryptase.
Instead, they are looking for a change in tryptase during a flare. The standard suggests to first get a baseline on a GOOD day. Then on a BAD mast cell day, get another test.
If your tryptase goes up 20% + 2 points from your baseline, then it’s considered a positive tryptase reading. Even if the tryptase level is still within normal ranges.
Now here’s another area where I think people get confused about tryptase.
If these baseline levels are considered high, that more likely indicates Mastocytosis or Hereditary Alpha Tryptasemia (HaT). HaT is a genetic problem that causes too much tryptase to be produced.
But remember, that while Mast Cell Activation Syndrome (MCAS) can occur with Mastocytosis or Hereditary Alpha Tryptasemia, these are all different conditions.
This is why according to many researchers, tryptase is not the most important marker that can indicate MCAS.
Do You Really Need a Diagnosis?
Currently we only have a handful of markers that can be tested. Yet, we know mast cells can release over 1000 mediators!
So, a question I keep coming back to is this – What if the mediators that can be tested for aren’t the ones your mast cells happen to be over releasing that day?
MCAS research is still a cutting-edge field. But with time I believe research will allow us to understand more about these questions.
But whether you do or don’t get positive results in your MCAS testing, you want to look for the root causes of your overactive mast cells.
So, what if you are one of the many people who can’t get a diagnosis?
Well, to me, the most important question is this – How are you going to feel better?
And to answer this question you need to ask another question – What is it that all these issues are really stemming from?
That’s where we get back to looking at the root causes. This is the approach we take in the Mast Cell 360 clinic.
That leads me to myth #7. Many people may say medication is the only way to feel better.
Read more to learn why this is also a myth.
Myth #7: Medication Is the Only Way to Address Mast Cell Activation Symptoms
In many cases, medication is essential to healing. And it can provide you with the relief from your MCAS symptoms that your body needs.
Both antihistamines and mast cell stabilizers can be beneficial for some. In many cases, these are two different things. But Ketotifen is unusual because it does both.
Ketotifen is an H1 blocker (blocks a histamine receptor known as H1) that has been shown to help stabilize the mast cells.
H1 blockers are medications typically used as antihistamines. They can help relieve many allergy-type symptoms.
These types of symptoms like itching, runny nose, and wheezing (to name just a few) can also be common with Mast Cell Activation Syndrome or Histamine Intolerance.
Other H1 blockers that may be helpful for some people include:
- Loratadine (Claritin)
- Fexofenadine (Allegra)
- Cetirizine (Zyrtec)
These are second-generation antihistamines. Second-generation antihistamines are considered safer long-term than first-generation antihistamines.
Other medications that may be helpful are H2 blockers like:
- Cimetidine (Tagamet)
- Famotidine (Pepcid AC)
Remember, histamine release can trigger the mast cells. So, getting that histamine response down can be helpful in calming the mast cells, too.
Related Article: The Best Antihistamines for MCAS and Histamine Intolerance
But even when needed, I see medications as only one part of addressing MCAS.
It’s also important to look at root causes.
You might think of it like this. If your house has a leaky roof, you can put buckets under the leak to catch any rainwater coming in from outside.
That will take care of water getting all over your floor.
But ultimately, you still need to fix the roof.
So, medications are one way to help control your symptoms. But you still need to look at what’s causing those symptoms to begin with.
Addressing your root causes is an important part of reversing MCAS.
We listed some of the major root causes we see in the Mast Cell 360 practice under Myth #3 above.
And you can sign up below for your free report on the 7 most common root causes.
Next, when it comes to feeling better, medications aren’t the only thing that can help, even though some people may say otherwise. Keep reading to learn more.
Myth #8: Supplements Can’t Help with Mast Cell Activation Syndrome and Histamine Intolerance
There are many ways you can support your health. Including supplements.
If you’ve heard supplements can’t help with Mast Cell Activation Syndrome or Histamine Intolerance, you’ve heard another popular myth.
Fortunately, this isn’t true. There is an extensive amount of research on histamine lowering and mast cell stabilizing supplements.
Here are a few of the best-known mast cell stabilizing supplements:
Quercetin
Quercetin has been shown to work as a mast cell stabilizer.
I find the form Alpha-Glycosyl-Isoquercitrin is the best absorbed. This means less is needed.
You can also get 15% off anything at Fullscript anytime when you register with our link. If you don’t have an account already, it’s free and you just enter your email address to sign up. It never costs you more and your Fullscript purchase helps support Mast Cell 360 free online resources.
Related Article: the Best Quercetin Supplements for Histamine Intolerance and MCAS
Baicalin
Baicalin may also be called Chinese skullcap. Don’t confuse this with American skullcap. They are very different.
If you try this, be sure to get Chinese skullcap (baicalin).
Chinese skullcap (baicalin) is a very effective mast cell stabilizer. I’ve had good experiences with this supplement when used for reducing mast cell related inflammation.
It can be hard to find Chinese skullcap, though.
This is the version we use in the Mast Cell 360 practice. It’s Chinese skullcap Extract (baicalin).
Use Coupon Code MASTCELL10 for 10% off!

Perilla Seed Extract
Perilla seed extract comes from a type of herb, perilla, used in Korean cooking.
It’s one of my favorites.
Perilla seed is high in apigenin, luteolin, and rosmarinic acids.
Research has shown these actions and properties:
- Reductions in histamine and the mast cell cytokine TNF-a
- Inhibiting inflammation
- Reductions in skin allergic reactions
- Improvements in respiratory symptoms
Related Post: Why Perilla Seed Extract Is the Mast Cell Supporting Supplement You’ve Never Heard About
Holy Basil
Holy Basil is also known as Tulsi.
It can be very effective for lowering the body’s stress response.
Stress on the body can be anything that knocks your body off balance.
Stressors can be physical, psychological, or chemical, just to give you a few examples.
I use a Holy Basil Tulsi supplement and the Tulsi Tea from Kauai Farmacy regularly. With both, I’ve had great results in inflammation reduction and feeling calmer.
Kauai Farmacy is very high-quality tea. Their Tulsi (Holy Basil) tea is delicious!
They harvest and ship in about a week. This makes it the lowest histamine and very fresh. Almost as good as plucking it from your own garden!
Use code MASTCELL360 to save 15%!

Boswellia
Boswellia is an extract of frankincense resin. I’ve used it in these two forms for MCAS:
Boswellia (Frankincense) Essential Oil
I’ve had good results using this essential oil to reduce inflammation and stabilize mast cells. If you use oils be sure to use a pharmaceutical grade ones (such as Rocky Mountain Oils).
Dilute frankincense with a carrier oil before applying it to your skin.

I’ve also had good results using Boswellia as a supplement for the same anti-inflammatory and stabilizing benefits.
Here is my favorite.
Remember, you can also get 15% off anything at Fullscript anytime when you register with our link. If you don’t have an account already, it’s free. It never costs you more and your Fullscript purchase helps support Mast Cell 360’s free online resources.
Vitamin C
Vitamin C has been shown to contribute to immune defense. It supports your body’s cellular functions in the innate and adaptive immune system.
And vitamins, like vitamin C, have been shown to have a protective effect on the body’s immune cells.
I’ve found vitamin C can help reduce my mast cell reactions, especially after exposure to a trigger.
However, many people with MCAS react to ascorbic acid because it is usually made from fermented corn.
These are 2 I’ve had good luck with:
I love camu camu because it’s not made from fermented corn. And it’s a food-based option.

Magnesium Ascorbate by Allergy Research Group
I’ve also had very good luck with this form of vitamin C. It is a buffered, non-acidic form of vitamin C, and is not fermented or from corn.
And if you have Salicylate Intolerance, this may be the better option for you since camu camu is high salicylate.
Related Article: Low Histamine Vitamin C
If any of these supplements are new to you, consider starting with just a few drops or sprinkles.
You can add them to water in very small amounts. If tolerated, you can slowly increase the amount.
Do you need help finding which supplements would be best for you?
Check out my Top 8 Mast Cell Supporting Supplements Master Class.
Now that you’ve read about some MCAS myths, you may want to look more deeply at symptoms of Mast Cell Activation Syndrome.
Are these symptoms something you’ve attributed to something else before because you didn’t think they could be related to MCAS?
A Deeper Look at Symptoms of Mast Cell Activation Syndrome
MCAS has been mystifying for practitioners for years because the symptoms can look very different person to person.
This is because mast cells are in every part of your body except your retina.
The symptoms you end up with depend on where the mast cells are dysregulated. Is it your skin mast cells? Your gut mast cells? Your brain mast cells?
Let’s start with a brief look at what mast cells are. This will help you understand why MCAS symptoms are so varied.
How Mast Cells Cause Symptoms
Mast cells are white blood cells. They are an important part of your immune system.
They are initially produced in your bone marrow. But mature mast cells aren’t found only in the bone marrow.
They are found in almost every part of your body.
All these mast cells have receptors. You could think of receptors as first responders. They respond to everything in and around your body.
They respond to everything from viruses and bacteria to chemicals and temperature.
Part of those responses can be the release of chemicals called mediators. These mediators play different roles in the body. They are very important in fighting infection and healing.
Why There Are Many Types of Symptoms
Here’s why it’s important to know that mast cells are in almost every part of your body.
Because mast cells are throughout your body, MCAS symptoms can occur in any of your body systems.
Which systems are affected depends on:
- The location of the mast cells being affected
- The receptors being triggered
- The mediators being released
With MCAS, we look for at least 2 body systems being affected. This is also referred to as being multi-systemic.
That’s the first clue – having symptoms in 2 or more systems of the body.
However, you should note that sometimes when 1 system has severe symptoms, it’s easy to overlook symptoms in other systems.
For example, you know that diarrhea and abdominal pain shouldn’t be happening every day. Those symptoms stand out.
But what about chronic sneezing or a runny nose? You may think it’s dust or an allergic reaction to something in your environment. But it could be related to MCAS.
In that case, you’d have both digestive and respiratory system symptoms.
But what about chronic sneezing or a runny nose? You may think it’s dust or an allergic reaction to something in your environment. But it could be related to MCAS.
The symptoms of MCAS vary widely.
So, it’s very important to talk with your provider about your symptoms. You want to rule out any other issues that may be life-threatening or that may need medical attention.
And some reactions may be anaphylactoid or anaphylaxis reactions. These are serious. Always be sure to contact your provider with any new or worsening symptoms.
But if you are like I was, your “strange symptoms” might be a mystery.
Does your bloodwork look fine?
Do you have urinary pain, but your culture comes back clear?
Maybe you’ve heard this – “You don’t look sick.” I heard that one a few times myself.
If so, you’ll want to learn more about Mast Cell Activation Syndrome.
Here at just some of the different symptoms you might have.
Symptoms in Different Body Systems
Do you have food, drug, environmental, or chemical sensitivities?
What about chronic inflammation?
Those are two symptoms that could be indications you have MCAS.
Mast Cell Activation Syndrome symptoms have been misunderstood for a long time.
Simply put, MCAS is a multi-systemic inflammatory disorder. And you can have it with or without allergies, anaphylaxis, or hypersensitivities.
Below, you’ll find more symptoms that affect different organ systems.
Cardiovascular System (Heart) Symptoms
A lot of the following heart-related symptoms can be related to MCAS.
But sometimes they can also be symptoms of something more serious. So, you’ll need to make sure those are ruled out with a healthcare practitioner. And, if you are feeling any new or worsening symptoms, it’s important to see your provider right away.
Some cardiovascular symptoms of MCAS can include:
- Feeling faint
- Passing out or fainting
- Chest pains (tightness of the chest)
- Fast heartrate
- Heart palpitations
- Dizziness or lightheadedness
- Low blood pressure
Digestive System Symptoms
The digestive system includes organs like your stomach and intestines. But it also includes your mouth. Your lips, tongue, and throat are all part of your digestive system, too.
Here are some common symptoms you might experience with your digestive system if you have MCAS:
- Mouth burning
- Trouble swallowing
- Throat tightness
- Gum inflammation
- Diarrhea
- Constipation
- Cramping
- Abdominal pain
- Irritable Bowel Syndrome
- Nausea
- Vomiting
- Reflux
- Bloating
- Food sensitivities
Integumentary System (Skin, Nails, Hair) Symptoms
Did you know that skin is the largest organ you have? I had a lot of skin symptoms related to MCAS.
And like you read, mast cells are almost everywhere in the body.
There were times I even felt like my hair hurt!
What symptoms related to skin, nails and hair have you experienced?
Here are a few to be aware of:
- Angioedema (swelling under the skin)
- Aermatographia (persistent redness or white marks after scratching)
- Urticaria (red, itchy welts)
- Flushing
- Itchiness
- Hives
- Rashes
- Bruising easily
- Burning sensations
- Slow healing of skin wounds
- Rosacea or reddish complexion
- Pale complexion
- Psoriasis
- Eczema
- Hair loss
Nervous System (Brain, Nerves) Symptoms
Working on my nervous system was a game-changer for my healing. I’ve had several of these types of a-ha moments on my healing journey.
Mold Toxicity is a major contributor to MCAS. And it can affect the nervous system in a big way.
That is one way you can get the over-responsive “haywire mast cells” that seem to cause negative reactions to everything, both good and bad.
Here are some symptoms that can indicate nervous system dysregulation from MCAS:
- Brain fog
- Short-term memory issues
- Trouble recalling words
- Headaches
- Migraines
- Depression
- Nerve pains
- Trouble focusing
- Anxiety
- Insomnia
- Dizziness
- Tinnitus
- Numbness
- Sweating
- Unusual temperature changes
- Tingling and numbness in arms and legs
- Other neurological symptoms like seizures
Respiratory System (Lungs, Sinuses) Symptoms
When the mast cells in your respiratory system are affected, you can get all kinds of different systems related to your lungs and sinuses.
Here are a few common symptoms of MCAS in the respiratory system:
- Congestion
- Coughing
- Shortness of breath
- Wheezing
- Asthma
- Increased mucous production
- Postnasal drip
- Sinus congestion
- Frequent throat clearing
- Sinus and/or nasal swelling
- Nasal polyps
Visual System (Eyes) Symptoms
Mast cells are even found in the eyes!
Do you have any of these symptoms of MCAS related to your visual system?
- Eye pain
- Redness
- Trouble focusing
- Inflammation
- Blurry vision
- Itchy, watery, or irritated eyes
Reproductive System Symptoms
So many times, women are told that their period pain is “normal.” It’s unfortunate because in some cases, painful periods are a symptom of MCAS.
And it can be addressed.
Here are some other conditions that may be related to Mast Cell Activation Syndrome:
- Endometriosis
- Painful periods
- Infertility
- Hormonal imbalances
Urinary Tract Symptoms
Have you had issues when you urinate?
Maybe you thought you had a UTI or other infection. But your bloodwork and cultures came back normal.
This happened to me on more than one occasion. It turns out these symptoms can also be related to MCAS.
Do you have any of these urinary tract symptoms?
- Inflammation
- Burning
- Pain with urination
- Urinary tract infection type symptoms
Musculoskeletal System (Muscles, Bones, Joints, Tissues) Symptoms
Pain in my muscles and joints was one of my biggest struggles. At one point, I was so bad off that I needed a cane just to get to my bathroom down the hall.
I was even misdiagnosed with Rheumatoid Arthritis when I was in my thirties.
But once I addressed MCAS and some of the food sensitivities underlying my mast cell activation, like Oxalate Intolerance, many of these joint and muscle issues went away.
I no longer need a cane to get around. I can even exercise normally and go on hikes!
Are any of these symptoms sounding familiar to you?
- Osteoporosis and Osteopenia
- Arthritis that moves around
- General muscular and bone pain
- Hyperflexible joints
- Degenerative disk issues
Related Article: What Is Oxalate Dumping?
Conditions Related to MCAS
There are a number of other conditions that may be related to MCAS, too. I was told I had at least a quarter of the ones listed below.
Now, you might have these conditions without MCAS symptoms, too.
Mast Cell Activation Syndrome isn’t the cause of all of these conditions. But it may be related in some instances. And you may get misdiagnosed, like I was.
My misdiagnoses meant I wasn’t addressing the big picture or root causes. It was like using a bandage when I needed a cast!
The related conditions are:
- Fibromyalgia
- Chronic Fatigue
- Interstitial Cystitis
- Crohn’s Disease
- Type 2 Diabetes
- Ehlers-Danlos Syndrome (EDS)
- Postural Orthostatic Tachycardia Syndrome (POTS)
- Autism Spectrum Disorders
- Autoimmune diseases
- Rheumatoid Arthritis
- Lupus
- Hashimoto’s Thyroiditis
- Guillain-Barré Syndrome
- Graves
- Sjogren’s
- Multiple Sclerosis
After looking at these symptoms and conditions, do you think you may have MCAS?
One Last Note on Mast Cell Activation Syndrome Symptoms
Unfortunately, there is still so much misinformation about Mast Cell Activation Syndrome out there.
Having some insights into the most common myths will help you understand your MCAS symptoms a great deal!
How many of these myths had you heard already?
Most people I talk to have heard at least 1. Usually, it’s even more. Good information is part of the challenge of navigating a condition that still isn’t fully understood or recognized.
Here’s one final myth for you.
Myth #9: Following an Aggressive, Standard Protocol Is the Only Way to Wellness
Not true.
You’ve already read how looking at your genes can show you that what you need may be very different than what someone else needs.
With MCAS, you need to know what to do AND you need to know the right time to do it.
Introducing something too soon can set you back further.
Onboarding something at too high a dose may cause reactions.
If you’ve tried other protocols that haven’t worked, you likely need a gentler, more tailored approach.
That’s exactly what the MC360™ Method does for you.
It’s already helped hundreds of clients in the Mast Cell 360 clinic get their lives back. You can learn more about this starting with my Top 8 Mast Cell Supporting Supplements Master Class.
Your key takeaway from this course is how to take the right supplements, in the right order, for you!
But most of all, I want you to know that if you do have MCAS, there is hope for you to get your life back.
What symptoms of Mast Cell Activation Syndrome do you suffer from? What myths did you believe before reading this? Tell me in the comments below!
More Mast Cell Activation Syndrome Basics
- Do You Have One or Both? Histamine Intolerance vs MCAS (Mast Cell Activation Syndrome)
- What Is MCAS?
- Mast Cells and Mast Cell Activation Syndrome 101
- Low Histamine Foods List for MCAS and Histamine Intolerance
- How to Customize Your MCAS Flare Up Plan
Some links in this website are affiliate links, like Amazon, which means Mast Cell 360 may make a very small commission if you purchase through the link. It never costs you any more to purchase through the links, and we try to find the best deals we can. We only recommend products that we love and use personally or use in the Mast Cell 360 practice. Any commissions help support the newsletter, website, and ongoing research so Mast Cell 360 can continue to offer you free tips, recipes, and info. Thank you for your support!
References
Afrin, L., Dr. “Presentation, Diagnosis, and Management of Mast Cell Activation Syndrome.” Mast Cells: Phenotypic Features, Biological Functions and Role in Immunity. Nova Science, 2013. 155-232
Afrin, L. B., et al. (2020). Diagnosis of mast cell activation syndrome: a global “consensus-2”. Diagnosis (Berlin, Germany), 8(2), 137–152. https://doi.org/10.1515/dx-2020-0005
Afrin, L. B., et al. (2016). Often seen, rarely recognized: mast cell activation disease – a guide to diagnosis and therapeutic options. Annals of Medicine, 48(3), 190–201. https://doi.org/10.3109/07853890.2016.1161231
Anogeianaki, A., et al. (2010, October). Vitamins and Mast Cells. International Journal of Immunopathology and Pharmacology, 23(4), 991–996. https://doi.org/10.1177/039463201002300403
Boyden, S. E., et al. (2016). Vibratory Urticaria Associated with a Missense Variant in ADGRE2. The New England journal of medicine, 374(7), 656–663. https://doi.org/10.1056/NEJMoa1500611
Carr, A. C., & Maggini, S. (2017). Vitamin C and Immune Function. Nutrients, 9(11), 1211. https://doi.org/10.3390/nu9111211
Hirano T., et al. Luteolin, a flavonoid, inhibits AP-1 activation by basophils. Biochemical and Biophysical Research Communications. 2006;340:1-7
Jarisch, R., et al. (2014). Impact of oral vitamin C on histamine levels and seasickness. Journal of vestibular research : equilibrium & orientation, 24(4), 281–288. https://doi.org/10.3233/VES-140509
Jennings, S., et al. (2014). The Mastocytosis Society survey on mast cell disorders: patient experiences and perceptions. The journal of allergy and clinical immunology. In practice, 2(1), 70–76. https://doi.org/10.1016/j.jaip.2013.09.004
Johnston, C. S., Martin, L. J., & Cai, X. (1992). Antihistamine effect of supplemental ascorbic acid and neutrophil chemotaxis. Journal of the American College of Nutrition, 11(2), 172–176
Kimata, Shichijo, Miura, Serizawa, Inagaki, & Nagai. (2000, April). Effects of luteolin, quercetin and baicalein on immunoglobulin E-mediated mediator release from human cultured mast cells. Clinical &Amp; Experimental Allergy, 30(4), 501–508. https://doi.org/10.1046/j.1365-2222.2000.00768.x
Krystel-Whittemore, M., Dileepan, K. N., & Wood, J. G. (2016, January 6). Mast Cell: A Multi-Functional Master Cell. Frontiers in Immunology, 6. https://doi.org/10.3389/fimmu.2015.00620
Makino, T., et al. (2003). Anti-allergic effect of Perilla frutescens and its active constituents. Phytotherapy research : PTR, 17(3), 240–243. https://doi.org/10.1002/ptr.1115
Makino, T., et al. (2001). Effect of oral treatment of Perilla frutescens and its constituents on type-I allergy in mice. Biological & pharmaceutical bulletin, 24(10), 1206–1209. https://doi.org/10.1248/bpb.24.1206
Molderings, G. J., Brettner, S., Homann, J., & Afrin, L. B. (2011, March 22). Mast cell activation disease: a concise practical guide for diagnostic workup and therapeutic options. Journal of Hematology &Amp; Oncology, 4(1). https://doi.org/10.1186/1756-8722-4-10
Prakash, P., & Gupta, N. (2005). Therapeutic uses of Ocimum sanctum Linn (Tulsi) with a note on eugenol and its pharmacological actions: a short review. Indian journal of physiology and pharmacology, 49(2), 125–131.
Shin, T. Y., et al. (2000). Inhibitory effect of mast cell-mediated immediate-type allergic reactions in rats by Perilla frutescens. Immunopharmacology and immunotoxicology, 22(3), 489–500. https://doi.org/10.3109/08923970009026007
Siddiqui M. Z. (2011). Boswellia serrata, a potential antiinflammatory agent: an overview. Indian journal of pharmaceutical sciences, 73(3), 255–261. https://pubmed.ncbi.nlm.nih.gov/22457547/
Weng, Z., et al. (2012, March 28). Quercetin Is More Effective than Cromolyn in Blocking Human Mast Cell Cytokine Release and Inhibits Contact Dermatitis and Photosensitivity in Humans. PLoS ONE, 7(3), e33805. https://doi.org/10.1371/journal.pone.0033805



I am not interested in buying supplements at this time. I have spent probably thousands of dollars on them trying to figure out what was wrong with me.
I just want to try to focus on diet for right now. How much of skullcap powder could I add to tea? I see you say start with sprinkles but what am I maxing at? Could I do the same with Camu Camu-add to tea or drink? Thank you for any advice you can offer. I appreciate your blog!
I know what you mean. General supplement recommendations rarely work for people with Mast Cell Activation Syndrome or Histamine Intolerance. I spent several thousand dollars on failed supplements before I learned how to target supplementation needs based on labs and genetics. This is where we get the best success. For skullcap and camu camu, it depends on the concentration you have. I would follow the package directions, and possibly experiment with a little more if you are doing well with them.
What about Pycnogenol®
Pycnogenol has been shown in research to have mast cell stabilizing properties. Pycnogenol is a brand name of pine bark extract. It is so effective, I used it in my MC Stabilizer formula. You can read more about pine bark extract properties in the formula sheet. Here is more info on the MC Stabilizer formula: https://mastcell360.com/supplements/
Hi Beth,
I was going to order the vitamin C product recommended above, but, when looking at the description on the manufacturers website, as I wished to ask them an other question, I
saw this stated under the vitamin c powder : «Source Materials: Ascorbic acid is derived from corn sorbitol. Sodium ascorbate is reacted from ascorbic acid and sodium bicarbonate. All ingredients are vegan and non-GMO.»
It looks like the ascorbic acid in the powder is derived from corn after all. What do you think about this, and what vitamin c supplement would you then recommend for someone sensitive, and with a sensitive gut? Hoping to get your opinion about this, as I am finding it somewhat difficult to know which vitamin c to try out. I am very low in vitamin c.
Secondly – I did read one of your other blog articles, and saw you mentioned coq10. Do you have a coq10 supplement for people low in this, to recommend not made through fermention? Or, do you find it Ok with the fermentation process in this regard?
Thank you!
Kindly, Ingrid
Unfortunately pycnogenol can be too astringent for some people, resulting in constipation and joint pain, among other thingsl
Hi Kelly,
I haven’t seen constipation with pycnogenol, but you are right, some people do react to it. With Mast Cell Activation, anything can be a trigger. Even very simple things. There isn’t a single supplement in my practice that everyone can tolerate. This is why it is critical to work with a health care practitioner and try new things very carefully.
I have just started taking chinese skullcap and camu camu and having really good results in just the past 3 days. However, I am reading on the internet that it can cause liver damage with other herbs. I do take other herbs. If I space them out, say 2 to 4 hours apart will that prevent liver damage? Or do you know if is it an issue even if you do that?
When I followed the link to the vitamin C you recommend, it says, “Ascorbyl palmitate is derived from corn dextrose fermentation and palm oil.” My impression from your post, though, is that this should offer a corn-free alternative for those who react. Did I misunderstand, or is there another product we should consider instead? Thanks.
Thanks for bringing this to my attention! It used to be made from tapioca. I added a different Vitamin C option above. Beth
I can’t even find a health care practitioner who can help me and diagnose if I have more than a histamine intolerance. A physician agreed to have my histamine level tested, which was high off the range, but he said there is not much known about it, and just gave me scripts for antihistamines and an epi pen. I search online myself and find people like you, spend more money than I have on supplements recommended, all trial and error. Dietary changes have helped some, and taking DAO enzyme has helped the most. How do I go about getting testing for more than the histamine? For mast cell, etc. ? Thank you.
Hi Peggy. Unfortunately, the testing for Mast Cell Activation Syndrome is fairly unreliable at this point in time. I recommend people rule out other conditions with their physician. And then also take a look at the symptom survey here: https://mastcell360.com/do-you-have-more-than-just-histamine-intolerance-take-the-mast-cell-activation-syndrome-symptoms-survey/
Just an FYI as I looked into a tapioca based Vitamin C (as ascorbic acid) for my MCAS daughter. I called the manufacturer and they confirmed it was derived by a fermented process. No corn, but fermentation, so it would be high in histamine and a no go for her unless we wanted to risk a reaction. We avoid fermented products or bi-products at all costs.
Thank you for all your information and helping the MCAS community!
Thanks so much, Nichole! Which brand was it? That info could really help a lot of people. Looking forward to hearing back from you.
Hi Beth. I notice you don’t mention tyramine intolerance as many of the issues MCAS folks can have as I know I have that and I think there are so many with migraine symptoms that also have never tried the low tyramine low histamine elimination diet to see if they improve without Tyramine triggers. I hope you bring this to light some and I am interested in working with you in the near future on my health issues ! thank you for this great blog!
Hi Sue Ann. Thanks so much for reading! I’m really glad you enjoy the blog. The low histamine diet on the website is also low tyramine. Histamine is a type of tyramine, and a low histamine diet includes tyramine triggers as well as other types of histamine triggers and liberators. Hope that helps!
I appreciate the information you put out there but I have to be honest …this will terrifies me! I don’t even know if I actually have MCAS but reading about all these triggers and problems. Yikes. Very overwhelming!
Jill,
I know it can be overwhelming. It was overwhelming for me in the beginning too. Take a look at the Symptoms Survey here: https://mastcell360.com/do-you-have-more-than-just-histamine-intolerance-take-the-mast-cell-activation-syndrome-symptoms-survey/
If you think you have Mast Cell Activation Syndrome, the most important thing is just to keep taking baby steps. It will start to become less overwhelming with time.
Hi Beth,
Just wondering which of the supplements you mentioned above are suitable for fertility / if you are trying to fall pregnant? I have read that Holy Basil for example should be avoided. Are there supplements that are suitable for fertility whilst working on Histamine/Mast Cell stabilising? If you don mind listing them that would be very helpful. I also need something that will regulate my irregular menstrual cycle if possible. I’m currently taking Vitex and was thinking of trying Shatavari (i’m not sure if Shatavari helps with histamine or not). If there is nothing else that regulates the cycles it would be great to at least know which of the Mast Cell stabilsing herbs are also safe for Fertility. Thankyou for such a wonderful blog and website 🙂
Hi Cindy,
I’m so glad to hear the website is helpful for you!
These are great questions! If you send us a message, we can connect you with someone who can help you with this.
https://mastcell360.com/contact/
Do you have any recommendations for Moringa Tea? Safety, etc?
Hi Judy
Moringa is often recommended as an anti-inflammatory superfood, but as healthy as moringa is, it’s not necessarily good for people with Mast Cell Activation Syndrome or Histamine Intolerance.
The reason for this is that moringa is high in oxalates. And oxalates can raise histamine levels.
You can read more about this and what to use instead here:
https://mastcell360.com/healthy-foods-to-avoid-when-you-have-mast-cell-activation-syndrome-or-histamine-intolerance/
Beth,
I just want you to know that your blog has helped me more than any practitioner I have had! I am working with a ND for mold toxicity but the level of detail you provide has been invaluable. I have taken your supplement class and highly recommend it to others. It turns out I have been dealing with Mast cell activation for over 10 years! I am finally clear of the mold but now have to figure out how to treat the mast cell stuff. Thank you so much for all of your detailed work on this blog! I would love to see you as a patient once you open up your practice to new patients. Got my fingers crossed as I am sure you are busy!
Hi Sara,
Thank you so much for reaching out. I am glad to hear you are finally clear of mold!
Hi Both, are any of these safe for slow COMT gene? I find sometimes Vitamin C and Quercetin increase my anxiety/cause shortness of breath. Are there any natural anti-histamines that are safe to use in such cases?
Hi Neha,
I don’t know if these will work for you since I don’t know your history, but these are usually better tolerated for over-methylators. Please be sure to talk with your practitioner with questions or concerns. If you decide these are right for you, start slowly and gradually build up. If you use the links below to set up a FullScript Account, you can get 15% off the FullScript orders. (does not apply to the DAO from Mast Cell 360 shop.)
BiCarb formula
https://us.fullscript.com/product_cards/70002/redirect?store_slug=mastcell360
All Qlear
https://us.fullscript.com/product_cards/77793/redirect?store_slug=mastcell360
DAO
http://www.mastcell360.com/shop
Perimine
https://us.fullscript.com/product_cards/62886/redirect?store_slug=mastcell360
Hi Beth, thank you for a very interesting and informative article.
My partner and I are hoping to start trying to conceive soon. I am currently wrangling with mast cell activation symptoms and was wondering if you know which of the above herbs are suitable to be on from a fertility perspective? I am also taking a combo of milk thistle, vitex, passionflower and shatavari, in the hopes of helping to regulate my cycle and for conceiving, although I’m not sure of their effect from a mast cell activation perspective? (hopefully positive!) Would you have any information on whether the above herbs you discussed are okay from a fertility perspective? And if the ones I’m using for fertility are okay from a mast cell activation perspective? If you have any information you could share at all or point me towards I’d be extremely grateful. Thank you as always for such fantastic and groundbreaking knowledge- I would be lost without this blog! Warmest regards and happy new year to your team. Dee
Hi Dee,
Thanks for reaching out to us. This is more than we can help guide you with online, but we are onboarding a fertility coach.
All the sodium ascorbate that I can find is derived from corn; even worse grown on aspergillus mould. I would also add mould and flouride to your brilliantly comprehensive list.
I think your website is great.
Hi Beth
The Chinese Skullcap extract Baicalin mentioned above by Liftmode contains Ascorbyl palmitate (Vitamin C) which you’ve mentioned in articles to avoid. Is there another brand you recommend?
Great website.
Hi Bob!
I’ve just double checked the listed ingredients for the Baicalin powder which you can find here: https://affiliate.liftmode.com/idevaffiliate.php?id=119&url=192
The powder doesn’t have ascorbyl palmitate. It may be possible that you got a link for the capsule instead. I will check our post here to make sure it is linking correctly. Thanks for reaching out!
Do you have any information on using LDN as part of treatment? I have Bartonella, mold, and MCAS and this therapy was recommended along with binders and anti inflammatory herbs. I would appreciate your opinion please. Thank you.
Hi Annette, Darin Ingels, ND discusses LDN in his interview on the Reversing Mast Cell and Histamine Intolerance Summit we hosted last month. If you missed it, you can purchase the summit at: https://mastcell360.com/AllAccess